Predicting Need for Intervention in Acute Necrotizing Pancreatitis Following Discharge
Guru Trikudanathan, MBBS, led researchers in a single-center study to develop a prediction model based on clinical metrics and imaging characteristics using a prospective data set meticulously collected for over ten years. The study was published in Pancreatolgy.

I think our study has further advanced the contemporary literature on this area by providing an extremely reliable prediction model which can guide discharge planning and judicious allocation of resources to patients who need closer follow up.
Guru Trikudanathan, MBBS
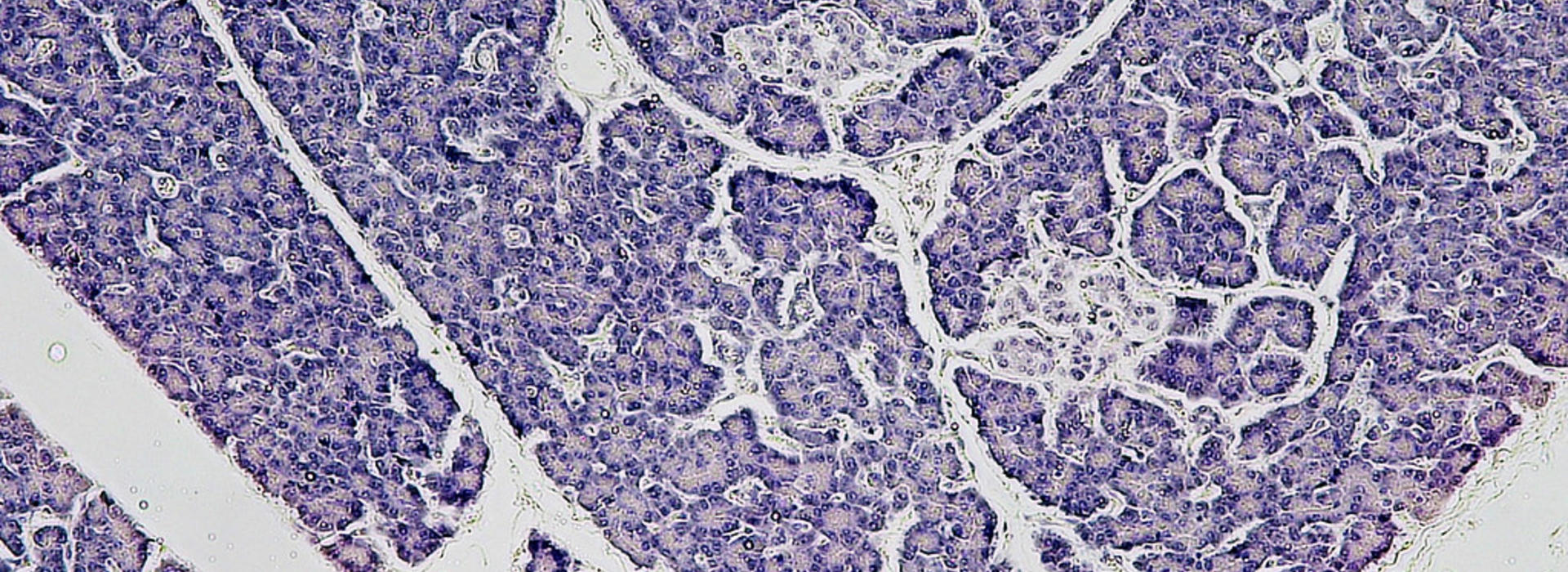
Acute pancreatitis is an inflammation of the pancreas which results in disabling abdominal pain and is a common cause of hospitalization. If the pancreas becomes inflamed, enzymes can leak into the pancreas and kill pancreatic tissue causing necrotizing pancreatitis. This complication poses a severe risk for infection and often warrants invasive endoscopic or percutaneous interventions. Identifying patients who will develop late symptoms and complications is advantageous, as they can benefit from closer surveillance.
Guru Trikudanathan, MBBS, led researchers in a single-center study to develop a prediction model based on clinical metrics and imaging characteristics using a prospective data set meticulously collected for over ten years. The study was published in Pancreatology.
This study enabled researchers to identify, upon admission, which patients hospitalized for necrotizing pancreatitis would likely require intervention following discharge. Transferred patients, white patients requiring total parenteral nutrition, necrotic collections larger than 6 centimeters, and fully encapsulated necrotic collections were more likely to undergo drainage or intervention after discharge. The model's receiver operating characteristic curve demonstrated an area under the curve of 0.88, suggesting a high degree of precision in the prediction model.
The study has further advanced the contemporary literature on this area by providing an extremely reliable prediction model which can guide discharge planning and judicious allocation of resources to patients who need closer follow up. Conversely, a predictive strategy also identifies patients likely to be managed conservatively and avoids unnecessary repeated cross-sectional imaging such as CT.
Multicenter studies and the leverage of artificial intelligence are needed to validate the prediction model further and integrate it into clinical practice.