Research Snapshot: Race Simulation Testing Recommended for Runners with Recurrent Heat Stroke
It’s no surprise that athletes are at risk for heat stroke during the blazing summer months; however, a recent case study from the University of Minnesota demonstrates that exertional heat stroke (EHS), a form of heat-induced illness, could still be life-threatening to athletes in cooler temperatures.
The research investigated a 30-year-old distance runner with a history of recurrent heat strokes while racing. A unique circumstance in relatively cool weather triggered a more extensive examination for cause, says William Roberts, M.D., M.S., author of the study from the Department of Family Medicine & Community Health in the University of Minnesota Medical School. The runner suffered from EHS despite the cooler temperature, highlighting the importance of race simulation testing for return-to-activity among athletes with a history of EHS.
The case study was published in Medicine & Science in Sports & Exercise.
Though the research focused on one runner’s condition, the results could influence the diagnoses of athletes with previous episodes of heat stroke.
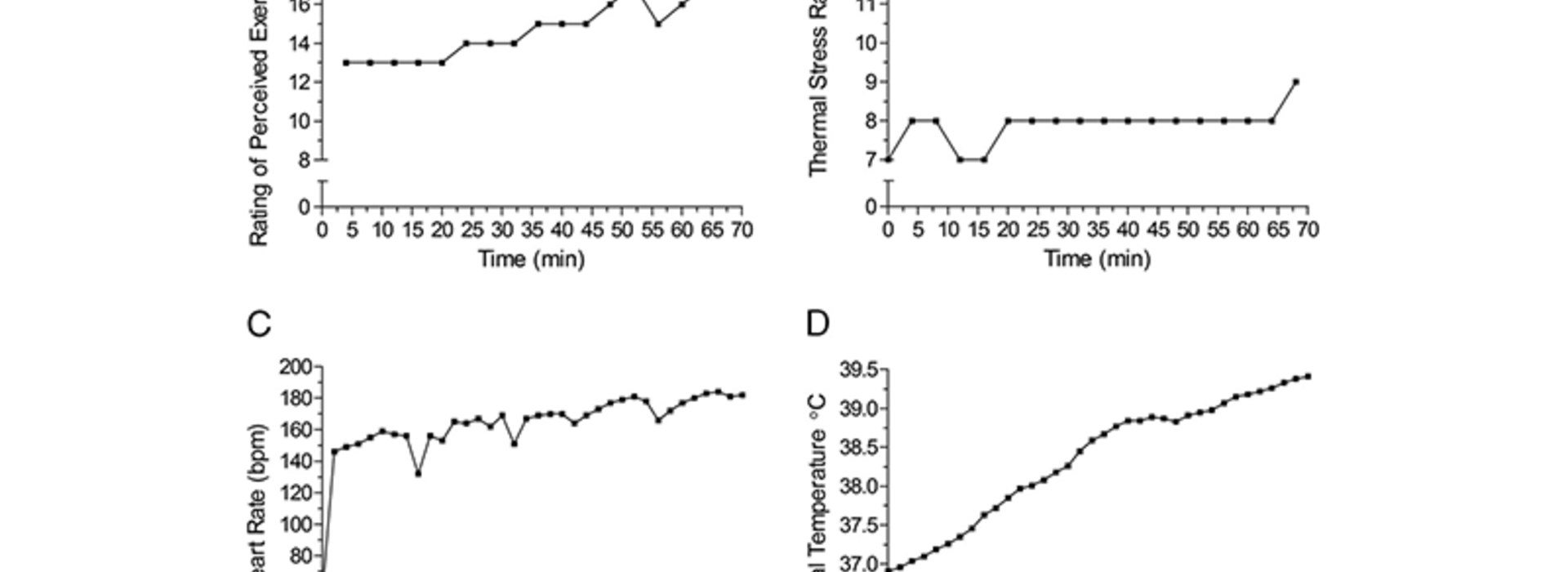
The heat tolerance test (HTT) is commonly used to screen for heat tolerance among patients, but it did not show a risk for heat stroke or EHS in the patient, leading experts to use a race simulation test. These findings from the research suggest additional tests should be considered among physicians to assist with preventative evaluations before patients return to activity.
“Testing in simulated race conditions revealed large sweat volume losses and large sweat sodium losses that likely contributed to his episodes of heat stroke,” said Roberts. “While dehydration is not a cause of most heat stroke cases, people who lose large volumes of sweat may be at increased risk like this runner.”
Roberts says hydration is necessary for managing body heat during physical activity, but drinking more than sweat loss could lead to fatal hyponatremia, a condition in which an excessive amount of electrolytes leads to low sodium levels in the bloodstream.
Controlling the salt and fluid intake during and after activity, the patient was able to run again.