2023 Advances in Learning Health System Sciences Conference
Held September 18-19, 2023 | Union Depot - Twin Cities, MN
The Conference
Thank you to everyone who attended our inaugural conference! This two-day event featured keynotes representing health services researchers, administrators, payers, and patient representatives, as well as a convening of expertise and insight on LHS topics ranging from real world data and implementation science to patient and community engagement. The educational content of this conference was eligible for AMA PRA Category 1 Credit TM and ACPE Contact Hours - learn more on the continuing professional development website.
If you are interested in becoming involved with CLHSS, learn more about membership.
A special thank you to SPH Alumnus Brian Osberg, MPH '86, and Jean Marie Hamilton for their generous gift to support Advances in Learning Health System Sciences Conference.

Congratulations to our Best Poster Award Winner!
Health and Wellness Among People Experiencing Housing Instability and Managing Cardiovascular Health: Qualitative findings from the CV-HOMES study
Drs. Kate Diaz Vickery, Rose Hyson, Andrew Busch
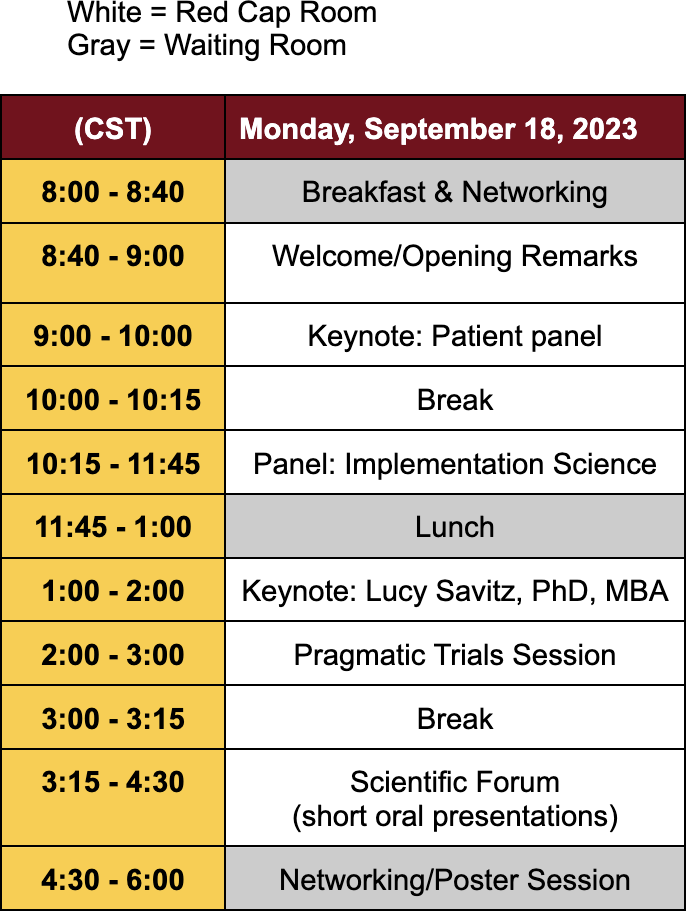
Monday, September 18, 2023
8:00 - 8:40 – Breakfast & Networking
Breaking Bread will be catering this event. Breaking Bread directly supports Appetite For Change, a community-led nonprofit using food as a tool to build health, wealth, and social change.
Location: Waiting Room
8:40 - 9:00 – Welcome/Opening Remarks
Genevieve Melton-Meaux, MD, PhD, FACMI (Director, CLHSS), and Timothy Schacker, MD (Executive Vice Dean, UMN Medical School), will start the conference with opening remarks.
Location: Red Cap Room
9:00 - 10:00 – Keynote: Patient Panel
Warren McKinney, PhD (VP for Equity in Research, Hennepin Healthcare Research Institute) will moderate the patient panel. The patient panelists will recount their experience with research in health care and discuss the value, opportunities, and gaps surrounding patient and family centered research.
Location: Red Cap Room
10:00 - 10:15 – Break
10:15 - 11:45 – Panel: Implementation Science
Debbie Pestka, PharmD, PhD (Research Scientist, CLHSS) will moderate this panel with the following key objectives: 1) Understand the fundamentals of implementation science; 2) Distinguish implementation outcomes from effectiveness outcomes; 3) Describe how implementation science can be applied within a health system. Each of the panelists will have an opportunity to share their perspectives, followed by a panel discussion, and Q&A.
| Joseph Gaugler Professor and Robert L. Kane Endowed Chair in Long-Term Care and Aging, University of Minnesota School of Public Health |
| Princess Ackland, PhD LP, MSPH Assistant Professor, Department of Medicine, University of Minnesota |
| Joel Farley, PhD Professor and Associate Head - Department of Pharmaceutical Care and Health Systems, University of Minnesota College of Pharmacy |
| Jennifer Ridgeway, PhD, MPP Associate Professor, Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery, Mayo Clinic |
Location: Red Cap Room
11:45 - 1:00 – Lunch
Breaking Bread will be catering this event. Breaking Bread directly supports Appetite For Change, a community-led nonprofit using food as a tool to build health, wealth, and social change.
1:00 - 2:00 – Keynote: Lucy Savitz, PhD, MBA
Lucy A. Savitz, Ph.D., MBA
Professor, Department of Health Policy & Management, University of Pittsburgh School of Public Health
Senior Innovation Advisor, UPMC Health Plan Center for High Value Health Care

Learning at the Intersection of Policy, Practice, and Research
Dr. Savitz will provide lessons learned over her 40-year career, working to advance health policy, healthcare delivery, and health services research. Examples of how embedded research has impacted at various scales in learning health systems will be used to illustrate challenges and emergent trends.
Location: Red Cap Room
2:00 - 3:00 – Pragmatic Trials Session
Joe Koopmeiners, PhD (Co-Director, RapidEval Program, CLHSS; Division Head, Biostatistics, UMN School of Public Health) will moderate this session. Dr. Koopmeiners will start with an overview of pragmatic trials followed by invited speakers presenting the development and implementation of pragmatic trials at various Minnesota health systems.
| Maya Peters, MPH Center for Learning Health System Sciences, University of Minnesota |
RapidEval Overview |
| Steven Fu, MD Director, Center for Care Delivery and Outcomes Research |
Veterans Affairs Programs |
| Lila Finney Rutten, PhD Mayo Clinic |
A stepped wedge cluster randomized trial to evaluate the impact of reminder/recall and audit and feedback on HPV vaccination |
Location: Red Cap Room
3:00 - 3:15 – Break
3:15 - 4:30 – Scientific Forum (short oral presentations)
Bronwyn Southwell, MD, (Integration Lead, Evidence Synthesis Program, CLHSS; Asst. Professor, Anesthesiology) will moderate this session consisting of accepted oral presentations from the conference call for abstracts. Each invited speaker will present for 12 minutes followed by a 3 minute Q&A.
| 3:15 - 3:30 | Leandria Albury University of Minnesota Medical School - Twin Cities |
Understanding Barriers to Lung Cancer Screening in a Minnesota Learning Health System Lung cancer remains the leading cause of cancer-related deaths in America. Recommended in 2013 by the United States Preventive Services Task Force (USPSTF) as a preventive service, lung cancer screening (LCS) remains poorly adopted. Only 5% of eligible persons in the United States (8% in Minnesota) completed recommended screening. The USPSTF recently expanded eligibility criteria in March 2021, which promises to reduce the lung cancer health disparities experienced by African Americans, American Indians, or Alaska Native Minnesotans and individuals of lower socioeconomic status. This expansion, combined with the positive impacts of early lung cancer detection on cancer survival rates, creates the perfect atmosphere to address the underutilization of LCS within learning health systems (LHS). By improving the delivery of LCS, these systems can mitigate low screening rates to directly impact care to patients, especially those experiencing lung cancer health disparities. Conducted within MHealth Fairview (MHFV), a multidisciplinary learning healthcare delivery system in Minnesota, this project used Human-Centered Design to understand existing barriers and facilitators of LCS. |
| 3:30 - 3:45 | Rebecca Brown Minneapolis Veterans Affairs Healthcare System |
Implementation of a Virtual Nurse Expert (VRN-e) Program to Improve Staff Retention, Nurse Sensitive Indicators, and Knowledge Acquisition Skills Retirements, burnout, growing demand with aging population have compounded the nursing workforce staffing shortages with a growing gap in experienced nurses in the workforce. (1, 2) Minneapolis VA Nurses optimize access to care for our Veterans using multiple modes of care delivery, including virtual platforms. Virtual care delivery was available across the United States healthcare system prior to the COVID-19 pandemic (3) and has now become a common mode of care delivery. Despite the gains of telenursing or virtual nursing in increasing access to care, there has been minimal impact of virtual care delivery on the underlying problem of nurse staffing and experience shortages.(4) Compounding this problem further is the lag and lack of systematic translation of scientific evidence into nursing practice. This problem is potentiated by information overload, lack of formal training in information acquisition, perpetual time constraints, and increasingly complex patient care. Clinical decision support systems (CDSS) have been one solution to acquire evidence-based information expediently, however, development of CDSS for nurses has been limited. Additionally, nurses, advanced practice providers, and physicians alike reportedly prefer a peer colleague over CDSSs or application-based resources. (5, 6) Peers are rich sources of information with mastery over multiple domains of knowledge and skillsets. Given the ongoing nursing shortage with personnel and experience, we are launching a virtual nurse expert program (VRN-e) to help bridge the experience gap, provide mentorship to newer staff to improve nurse burnout and retention, leverage unit-based quality data to inform care, teach knowledge acquisition skills to navigate the mass of educational resources available to nurses, and standardize procedures. Purpose: The VRN-e program aims to systematically extend the expertise of experienced nurses to their service units, fellow nurses, and patients to mitigate staff shortages and burnout and improve patient care and nurse retention. |
| 3:45 - 4:00 | Megan Reams HealthPartners |
Patient Reported Outcomes | Practice-Research Partnerships: Important and Feasible Policymakers and academics have been decrying the 17 years it reputedly takes for research results to be widely implemented in practice.1This “delay” in the translation of evidence into practice has been explained in part by researchers studying impractical solutions for clinically unimportant problems and in part by the drastic difference in goals, cultures, and timelines between research and practice. The issue became a national priority with the publication in 2001 by the Institute of Medicine’s “Crossing the Quality Chasm” report, followed in 2007 and beyond by suggestions and reports on a solution that has been called the “Learning Healthcare System.”2,3 As defined by the Institute (now National Academy) of Medicine, a learning healthcare system is “designed to generate and apply the best evidence for the collaborative healthcare choices of each patient and provider; to drive the process of discovery as a natural outgrowth of patient care; and to ensure innovation, quality, safety, and value in health care.” However, apart from a few large data-sharing or collection efforts and a few atypical health systems with researchers employed by the care system, the vast majority of patient care and research continues to be performed in two quite separate worlds, with limited interactions and very few truly joint projects. Even embedded researchers largely pursue studies that meet the goals of funders and researcher careers. Some of us whose careers have encompassed both research and practice have wondered if there isn’t an alternative for studies that focus on problems and goals that truly originate in patient care and contribute to both the current clinical situation and generalizable knowledge. This case report provides a very specific example of what can be done. |
| 4:00 - 4:15 | Luis Silva University of Minnesota |
Effectiveness and Safety of Tenecteplase versus Alteplase in Acute Ischemic Stroke in Selected Subgroups Acute ischemic stroke (AIS) is a leading cause of disability in the United States. (Tadi & Lui, 2022). As such, interventions that lead to better functional outcomes should be investigated thoroughly by clinical trials and confirmed by Real-World Data. Thrombolysis with alteplase (the “clot-buster”) is the only FDA-approved medical treatment for AIS. Tenecteplase (TNK) is a plasminogen activator derived from Alteplase with three amino acid substitutions that confer a favorable pharmacological profile, a longer half-life, and higher fibrin specificity, facilitating streamlined drug preparation and administration. Additionally, lower pricing of TNK makes it currently especially cost-effective. Pivotal AIS trials, including EXTEND-IA and NOR-TEST, have shown that TNK may be a safe and effective alternative to Alteplase and support its utilization in routine clinical practice. (Campbell et al., 2018; Logallo et al., 2017). On February 17, 2021, the M Health Fairview was one of the first health systems to implement the universal adoption of TNK to treat AIS. This study aims to elucidate the comparative effectiveness of these two medications on the healthcare population seen in this system. |
| 4:15 - 4:30 | Emily Hudson Minneapolis VA Medical Center |
Applying a Learning Health System Approach to Understand Multi-Level Stakeholder Needs for care of Veterans with Dementia Following Hospitalization Hospitalization is more frequent in persons with dementia and threatens their ability to live at home due to hospital-associated deconditioning and the emergence of challenging behaviors when exposed to an unfamiliar hospital environment. Alternative post-acute care models are crucial for Veterans with dementia to recover at home. One example is telerehabilitation, the technology for communication (e.g., phone, video) to support the delivery of rehabilitation services in the home. Yet a critical gap exists as current post-acute paradigms for Veterans with dementia tend to default to short-term rehabilitation in a nursing home. This study aims to identify the needs of Veterans with dementia, care partners, and rehabilitation clinicians when referring to or receiving home-based models of care following hospitalization--including telerehabilitation--to inform the implementation and adaptation of models to the post-acute context. Importantly, this study aligns with the Veterans Health Administration’s (VHA) vision to become a learning health system and priorities of enhancing access to and delivery of high-quality care that (1) leverages the use of technology and (2) honors Veterans’ preferences to live either at home or in the least restrictive environment possible. |
Location: Red Cap Room
4:30 - 6:00 – Poster Session
This session will take place in the Waiting Room and will be open to all attendees to interact with the poster authors and network into the evening. A four judge panel will review the posters during this session and deliberate to select a single recipient of "Best Poster Award", which will be announced at the opening remarks on September 19.
| Salman Ali University of Minnesota Medical School |
Disparities in No-Show Rates at Smiley's Clinic for English-Speaking vs. Non-English-Speaking-Patients |
| Samuel Boes University of Minnesota Stroke Research Fellowship |
TELECAST-2: Improving Stroke Care Disparities in Underserved Communities |
| Chloe Botsford CLHSS, DFMCH |
Fostering a Climate of Curiosity in Primary Care by Growing a Practice Based Research Network: A Process Description |
| Chloe Botsford CLHSS, DFMCH |
First Steps Towards Building a Climate of Curiosity Through a Practice Based Research Network at the M Health Fairview Andover Clinic |
| Nitin Ramanujam Chakravarthula University of Minnesota |
A Proposal for Accelerated and Improved Inpatient Stroke Evaluations with Cardiac CTA |
| Joey Dagher Hennepin Healthcare Research Institute |
Health, Homelessness, and Criminal Justice Lab: Meeting People Where They Are: Behavioral Health Studies in the Health, Homelessness, and Criminal Justice Lab |
| Elisheva Danan Minneapolis VA |
A Learning Health System Approach to Improve Cervical Cancer Screening in the VA |
| Zachary Davidson Hennepin Healthcare |
You Aren’t The Doctor I Saw Last Time: Improving Resident-Patient Continuity in an EM-IM Resident Clinic |
| Stuart Grande Health Policy and Management, UMN SPH |
A Simple Upstream Intervention to Establish Whole-Person care for Aging Adults with Subjective Cognitive Impairment: The About Me Care Card |
| Allison Gustavson Minneapolis VA Medical Center |
Applying i-PARIHS to Identify Emerging Innovations in Hospital Discharge Decision Making in Response to System Stress |
| Adam Kaplan Center for Care Delivery and Outcomes Research |
Clusters Based on Within-Treatment Symptom Trajectories as Predictors of Dropout in Treatment for Posttraumatic Stress Disorder and Substance Use Disorder |
| Martha Barnard & Matt Loth UMN; CLHSS |
A simulation study of the usefulness of overlap weighting based causal inference in a learning health system |
| Meghan Munger Gillette Children's Specialty Healthcare |
County variation in families of children with disabilities receiving TEFRA |
| Eduardo Osegueda University of Minnesota School of Public Health |
Applying the Consolidated Framework for Implementation Research (CFIR) to understand facilitators and barriers to optimizing inpatient sepsis care |
| Debbie Pestka UMN/VA |
Increasing Prescribing of Sodium-Glucose Cotransporter-2 Inhibitors Among Eligible Patients in the VA: A Targeted Pharmacist Intervention |
| Sripriya Rajamani School of Nursing, University of Minnesota |
Academic-Practice Partnership to Build Informatics Capacity in Public Health and Support move towards Learning Health Systems Model |
| Megan Reams HealthPartners |
An Implementation Science Approach to Identifying Factors that Influence Surgeon Decision-Making – On the Road to High Value Care |
| Karen Stalin University of Minnesota |
Improving Research Recruitment in Stroke Trials through Research Integration Training |
| Timothy Usset Minnesota Evidence-Based Practice Center/VA Maine Healthcare System/Physicians Wellness Collaborative |
Moral Injury and Occupational Functioning in Healthcare Workers |
| Katherine Vickery Hennepin Healthcare Research Institute |
Health and Wellness Among People Experiencing Housing Instability and Managing Cardiovascular Health: Qualitative findings from the CV-HOMES study |
| April Wilhelm University of Minnesota |
A Day-in-the-Life of Academic Family Medicine Scholarship/Research from a Harmonization Approach |
| Qi Zhang & Zach Henderson Fairview |
Transforming Harmonized and Consolidated Supplies Data in Surgical Data Mart |
| Jeanette Ziegenfuss HealthPartners Institute |
Convening Community Partners to Inform a Learning Health System |
Thank you to Helen Parsons (School of Public Health), Adams Dudley (Medical School, VA), Steve Dehmer (HealthPartners), and Rubina Rizvi (CLHSS) for serving on the judges panel.
Location: Waiting Room
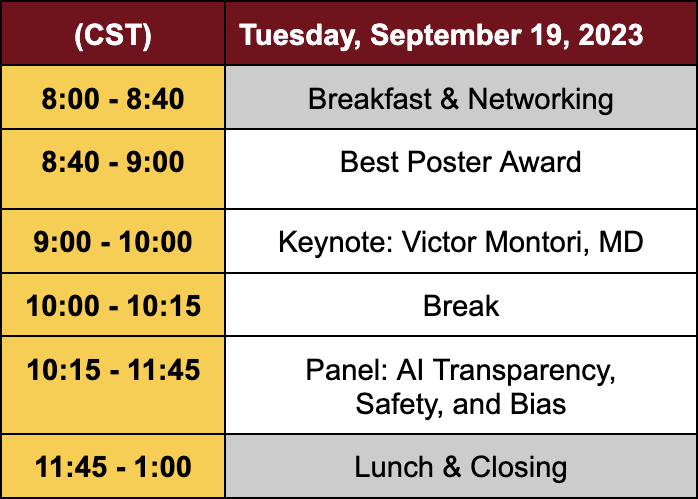
Tuesday, September 19, 2023
8:00 - 8:40 – Breakfast & Networking
Breaking Bread will be catering this event. Breaking Bread directly supports Appetite For Change, a community-led nonprofit using food as a tool to build health, wealth, and social change.
Location: Waiting Room
8:40 - 9:00 – Opening Remarks & Best Poster Award
Timothy Beebe, PhD, (Deputy Director, CLHSS) will give opening remarks and announce the Best Poster Award.
Location: Red Cap Room
9:00 - 10:00 – Keynote: Victor Montori, MD
Victor Montori, M.D.
Robert H. and Susan M. Rewoldt Professor of Endocrinology
Investigator, Knowledge and Evaluation Research Unit
Consultant, Division of Endocrinology, Department of Medicine
Mayo Clinic

The Clinical Encounter: From Black Box to Research Frontier
People in the healthcare system care and learn, fully realizing these roles when healthcare professionals interact with patients. The smallest unit of interaction is the clinical encounter. It is here that policies become practices, and practices contribute to outcomes. And yet, despite its centrality, the encounter remains a black box. To learn and care well, researchers must crack the box open, investigate it beyond "experience", and advance the science of care.
Location: Red Cap Room
10:00 - 10:15 – Break
10:15 - 11:45 – Panel: AI Transparency, Safety, and Bias
Chris Tignanelli, MD, MS (Co-Director, Program for Clinical AI, CLHSS; Assistant Professor, Surgery) will moderate this panel. Each of the panelists will have an opportunity to share their perspectives, followed by a panel discussion, and Q&A.
| Sabrina Hsueh, PhD, FAMIA Director of Ethical AI and External Innovation, Pfizer |
| Dennis Murphree, PhD Director, Digital Health and Artificial Intelligence | Mayo Clinic Dermatology |
| Phil Lindemann VP, Data and Research Informatics, Epic |
| Gyorgy Simon, PhD Scientific Co-Director, Center for Learning Health System Sciences Associate Professor, Institute for Health Infromatics, University of Minnesota |
Location: Red Cap Room
11:45 - 1:00 – Lunch & Closing
Breaking Bread will be catering this event. Breaking Bread directly supports Appetite For Change, a community-led nonprofit using food as a tool to build health, wealth, and social change.
Location: Waiting Room
Schedule at a Glance