University Researcher Determined to Enhance Understanding of Neck Pain
Neck pain is the third most common chronic pain condition in the U.S. and the fourth leading cause of disability worldwide, according to an article published in the Journal of the American Medical Association and corroborated by a number of other scientific papers. Arin Ellingson, PhD, is an assistant professor in the Department of Rehabilitation Medicine with an adjunct appointment in the Department of Orthopedic Surgery, and is determined to enhance our understanding of neck pain and improve treatment options.
Ellingson’s research project, “Intersegmental Dynamic Mechanisms of Neck Pain In Vivo,” a collaboration with the Department of Rehabilitation Medicine, was awarded a National Institutes of Health (NIH) R03 grant on June 9, 2019. Ellingson’s research centers around growing evidence that there is a biomechanical element to neck pain and will use state-of-the-art technology to provide new insight on movement dysfunction.
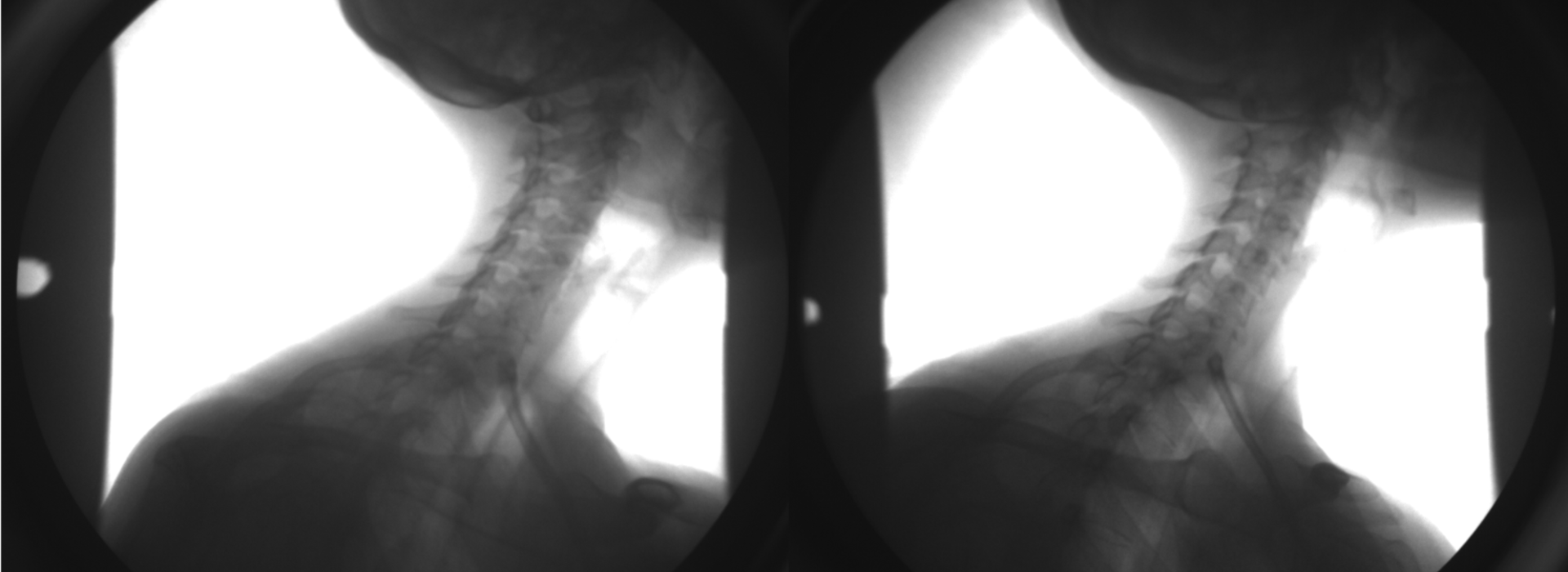
“One of the big reasons that I joined the faculty here is a piece of equipment called biplane radiography,” Ellingson explained. “It uses two x-ray sources to acquire simultaneous images so that we can actually reconstruct bone geometry in three dimensions during dynamic functional motion.”
A typical motion-capture system uses a camera and reflective markers which can be tracked by researchers.
“The big problem with the spine is that there’s a lot of soft tissue motion on top of the vertebral body that we’re trying to track,” Ellingson says. “Using the new device, we can get real-time 3D bony motion, which offers a lot of opportunity on top of traditional static imaging.”
Using traditional static imaging, patients are placed in the supine position in a CT or MRI scanner, not bearing any weight and not moving. The biplane radiography system gives the team the opportunity for the first time to understand how vertebrae move relative to one another. Ellingson says that the system was originally designed to be used in the lower extremities to understand knee motion and is now being used to understand more complex joints. There are roughly 18 such systems across the country.
So far, Ellingson has enrolled and collected data on one human subject, but is working to enroll 60 for the grant. He is seeking 20 asymptomatic individuals, 20 age and sex-matched individuals with mechanical neck pain, and 20 with cervical radiculopathy.
“One of the aims of this grant is to see if there’s any biomechanical mechanism for individuals with nonspecific mechanical neck pain,” he says. “We are also trying to enroll individuals with unilateral cervical radiculopathy (symptoms on just one side), to see if there are any differences in the neural foraminal space (space between the vertebrae that nerves travel through to other parts of the body), and then compare it to asymptomatic participants.”
Subjects perform planar activities (flexion/extension, bending, and rotation) as well as an activity called circumduction. During circumduction, the subject rolls their head around while their torso remains stationary to combine all planar activities.
“This movement in particular will help validate the way we test for cervical radiculopathy,” Ellingson explained. “We ask subjects if they have pain during the activity, where the pain is located, and see if that neural foraminal space is actually closing. It will give us some insight into how the pain is being generated.”
Ellingson added that some research suggests that individuals with mechanical neck pain have some spinal instability, so he is also gathering stability metrics from each spine. Ellingson has collaborated with orthopedists in the department to help with recruitment and interpretation of the clinical data. Associate Professor Jonathan Sembrano, MD, and Assistant Professor Christopher Martin, MD, are official collaborators on the grant.
“Although there are many studies evaluating neck motion, Dr. Ellingson's biplanar fluoroscopy technology would allow dynamic in vivo assessment of segmental cervical spine motion in different planes during functional active neck motion,” says Sembrano. “This would greatly enhance our understanding of changes in neck motion between painful and non-painful states, how people compensate for painful movements, which particular movements are limited, and whether and to what degree these motions are recovered after successful treatment.”
Martin added, “Arin’s work is helping advance the cutting-edge of orthopedic and spine science.”
The second part of the grant is collaborating with researchers from the computer sciences to create an interactive visualization environment.
“We will be taking all the biomechanical and clinical data and putting it into software to see what trends arise,” Ellingson explained. “Then we’ll use those trends and outcome variables to target subsequent projects where we will have an intervention, whether that be conservative or surgical treatment.”
The ultimate goal of the research is to develop an objective movement dysfunction-based tool that will better predict the best course of treatment for patients and perhaps allow earlier intervention.
“Dr. Ellingson's biplanar fluoroscopy investigating the patient’s kinematics gives him and our surgeons an exceptional means to link the disc’s physical properties with the patient’s spine motion,” says Joan Bechtold, PhD, professor and vice chair of research. “This combination is unparalleled worldwide.”
Future research will also focus on how individuals move following arthroplasty, arthrodesis, and other procedures. While the project is not yet conceivable as a clinical tool due to the amount of processing necessary to get meaningful data, the research may give insight into some of the mechanisms of pain generation and specific levels of movement dysfunction.