Hematopathology Builds on 50 Years of Bone Marrow Transplantations

It was half a century ago that University pediatrician and pathologist Robert Good and his clinical team performed the world’s first successful bone marrow transplant. The University has been at the forefront of bone marrow transplantation ever since. That gives LMP hematopathologists like Michael Linden plenty of opportunities to evaluate bone marrow transplant patients for evidence of minimal residual disease following transplant and solid organ transplant patients for post-transplant lymphoproliferative disorder (PTLD) following immunosuppression.
“Most of the patients coming for a bone marrow transplant have Non-Hodgkin lymphoma (NHL), Hodgkin lymphoma (HL), acute myeloid leukemia (AML) or myelodysplastic syndrome (MDS),” said Linden, who directs LMP’s Hematopathology Division. “We review their original diagnostic materials, confirm or refine the diagnosis, then test for residual disease after treatment.” Academic medical centers like the University that do a lot of solid organ transplants see many post-transplant patients with post-transplant lymphoproliferative disorder, a malignancy driven by the Epstein-Barr virus, because their immune system is compromised, he said.
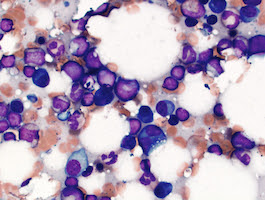
Linden and his fellow hematopathologists primarily serve the MHealth clinicians in two ways: by performing microscopic evaluation of blood, bone marrow, and tissue; and conducting sophisticated flow cytometry analyses. The Flow Cytometry Lab, directed by Elizabeth Courville, has three 10-color flow cytometry instruments. “We have the instrumentation and technical expertise to do moderate to high-complexity testing,” Linden said.
Laboratory Medicine and Pathology’s hematopathology team – Courville, Bartek Grzywacz, Linden, Pawel Mroz, Sarah Williams and Sophia Yohe -- is influenced by the volume of transplants at the University. For adults, they include transplants for myeloma, NHL, HL, and acute leukemia; for children, they include transplants for acute lymphoblastic leukemia and inherited disorders like Fanconi anemia and dyskeratosis congenita, conditions in which the University has gained a reputation for special clinical expertise.
“We’re an intermediate volume place,” Linden said. “Too small and you don’t get the breadth and volume to maintain or advance skills. If you’re very high volume and your focus is turnaround time you may not get as much time per case. I think we’re kind of in that sweet spot where we have really good expertise and enough volume and breadth to approach cases in an optimal way.
The hematopathology team holds a daily consensus conference where faculty, fellows, residents, medical students, and observers meet to discuss difficult diagnostic cases and try to arrive at the best consensus opinion for that patient. “It’s a working conference for the faculty to arrive at a diagnosis. We consult the World Health Organization “Blue Book” classification of tumors of hematopoietic and lymphoid tissues and review and discuss each case with its guidance,” Linden said. The consensus conference aims to provide a high-quality diagnosis for patients and also an exemplary learning opportunity for trainees. Two of Linden’s predecessors as LMP’s Hematopathology Division Director, Richard Brunning and Robert McKenna, were chapter authors of the World Health Organization Blue Book, helping to establish the prestige of University hematopathology world-wide. Linden highlights that fact plus the diverse education and specialty training of current faculty in his recruitment efforts.
“What I like to showcase about the group when interviewing candidates for either residency or fellowship is the pedigree of our training,” Linden said. “All six of our hematopathology faculty trained at different programs. Specialty training is a little bit different from one program to the next. So we have a variety of emphases based on a given faculty member’s training and previous experience. That complements the way we think about a case and approach it.”
If you have questions about how to refer a consult to our University of Minnesota Physicians Outreach Laboratories or about pricing, contact Laura Funches at 612-625-3949 or at lfunches10@umphysicians.umn.edu or contact the Hematopathology Division directly -- Kris Bergstedt at 612-273-5136 or at kbergst2@fairview.org.