Modeling Alzheimer’s disease and related dementias takes a major step forward
University of Minnesota researchers working with colleagues in the MODEL-AD Consortium and the Jackson Laboratory have taken a major step toward moving the genetics of Alzheimer’s disease (AD) and related dementias (ADRD) into experimental mice.
Advances in treatments for AD and ADRD depend on accurate and reliable mouse models that closely mimic the molecular and cellular processes and the resulting pathology in humans. Standard transgenic mouse models, widely used in the field, can mimic certain aspects of AD pathology but not AD genetics, which govern when the disease arises, how it develops, and who is susceptible.
 Laboratory Medicine and Pathology professor Michael Koob together with his research team and collaborators Adrian Oblak from Indiana University and Gregory Carter and Michael Sasner from the Jackson Laboratory have published “Gene replacement-Alzheimer’s disease (GR-AD): Modeling the genetics of human dementias in mice” in a special issue of Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association.
Laboratory Medicine and Pathology professor Michael Koob together with his research team and collaborators Adrian Oblak from Indiana University and Gregory Carter and Michael Sasner from the Jackson Laboratory have published “Gene replacement-Alzheimer’s disease (GR-AD): Modeling the genetics of human dementias in mice” in a special issue of Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association.
"Medical and long-term dementia care impose heavy burdens on patients, their families, and society, with cumulative financial costs Projected to grow from billions to trillions of dollars in the decades ahead."
The primary goal of Koob and his colleagues is “to develop mouse lines that model the genetics of AD/ADRD as closely as possible,” which they term Gene Replacement (GR)-AD. The project brings together Koob’s cutting-edge gene replacement technology, the Model Organism Development and Evaluation for Late-onset Alzheimer’s Disease (MODEL-AD) Consortium based at Indiana University, and the Jackson Laboratory (JAX) with its more than 13,000 experimental mouse strains.
With ongoing support from the National Institute on Aging (NIA), MODEL-AD was established in 2016 to accelerate AD/ADRD drug development by generating animal models that more closely resemble human characteristics of the disease. NIA is a key funder of Koob's research.
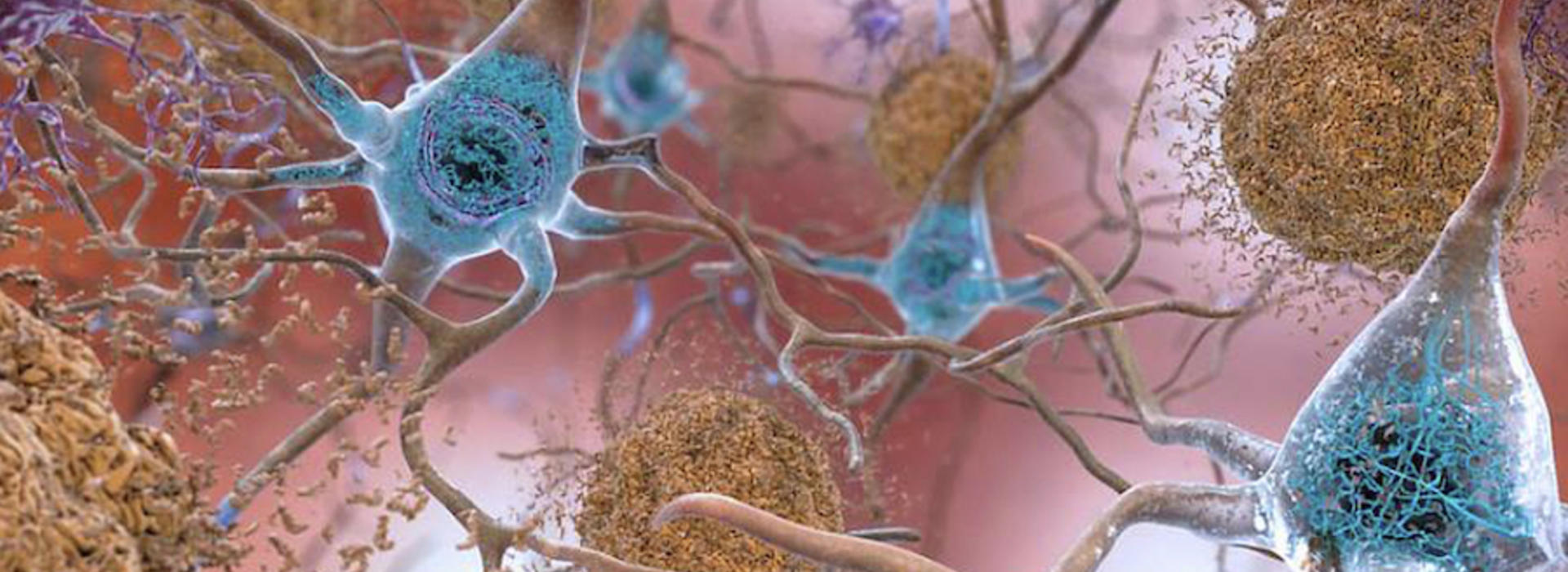
Koob’s laboratory has pioneered full human gene replacement in mice beginning with the gene for microtubule-associated protein tau (MAPT) in 2019. Mutations of tau lead to spaghetti-like neurofibrillary tangles in the brain, which are a common feature of AD and ADRD. Along with beta-amyloid plaques found in AD, mutated tau protein is a key target for therapeutic interventions designed to slow progression of AD and ADRD.
ADRDs include, among other conditions, frontotemporal dementia (FTD), Lewy body dementia (LBD), vascular contributions to cognitive impairment and dementia (VCID), and multiple-etiology dementias (MED). AD/ADRD patients typically share multiple genetic aberrations and the flawed proteins they produce, proteins that damage brain cells and inhibit their ability to function normally.
In their paper, the investigators provide an overview of the first 10 AD and ADRD-related human genes introduced into the mouse genome, replacing related mouse genes. In addition to tau genes, they include genes for the amyloid-beta precursor protein APP and alpha-synuclein. Accumulation of alpha-synuclein is a hallmark of many dementias including AD, FTD, LBD, MED, and Parkinson’s dementia.
In all, 27 AD and ADRD-related human genes have been introduced into mice thus far. The GR-AD project will develop mouse models with multiple mutated AD and ADRD human genes in a strategy to recapitulate what typically happens in patients. Each mutated strain model is accompanied by a matched control.
“There’s been a real lack of experimental systems that model this type of genetics,” Koob said, noting that transgenic mice typically carry a small amount of human DNA (cDNA) and do not produce the complete protein and its variants (isoforms) that full human genes produce. “Our goal is to move the power of the human genetics from the human into the mouse -- to mimic the genetics of human disease as closely as possible in mice.”
Replacing key mouse genes with full-sequence human genes, and in the corresponding location in mouse chromosomes with adjacent regulatory sequences, has never been done before in an effort to understand how a degenerative disease unfolds. Because the inserted human genes produce the corresponding human protein, investigators can track proteins associated with human dementia in mouse tissues, specifically in the brain and central nervous system. Mutated human tau genes in a mouse, for example, produce mutated human tau proteins – the tau tangles associated with pathology and neurodegeneration – in the mouse brain.
“With these models, it is now possible for the first time to do the human genetics of AD/ADRD in the mouse,” Koob said.
To accelerate adoption of the technology, “GR-AD models are being made available through the Jackson Laboratory mouse repository as soon as is practical for academic and commercial use without restrictions,” the authors write. Koob said six GR-AD mouse lines are currently available at JAX with six more in the process of being made available for wide distribution. Others will follow.
More than six million Americans are living with AD/ADRD dementias today. The number could more than double by 2060 barring the development of medical breakthroughs to prevent, slow or cure these diseases, according to the Alzheimer’s Association. Medical and long-term dementia care impose heavy burdens on patients, their families, and society, with cumulative financial costs projected to grow from billions to trillions of dollars in the decades ahead.