3D Modeling
CarePrints
The CarePrints program was established in 2015 as a way to help families better understand their child’s surgery to repair a congenital defect. Instead of using just standard CT or MRI images to try and explain the complex defects, the same data is used to generate a 3D model. This model is 3D printed and given to the family, allowing the surgeon to point out and explain each defect and how it is affecting the patient.
Virtual Reality
The Visible Heart® Laboratories prides itself for being at the forefront of cardiac visualization. This has led to the development of a virtual reality platform for anatomic learning. The platform was created using Unity3D software and custom C# scripts that allow users to navigate throughout the virtual environments and interact with the anatomical models. The anatomical models within the virtual environments are created from high resolution MRI and CT scans of actual human anatomies. This allows for the user to be immersed in highly detailed anatomical models that preserve the intricacies of the human anatomy.
Continue Reading
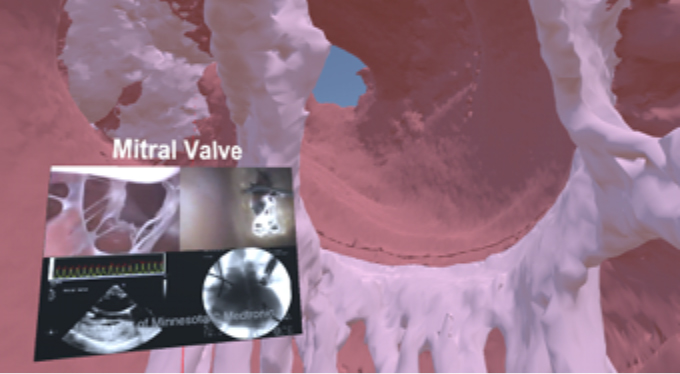
A user flying through the left ventricle of a human heart in virtual reality. The user is studying the mitral valve of the heart while viewing functional anatomical videos within the virtual environment to enhance their learning.
The virtual reality platform also encompasses the visible heart laboratories rich, fresh human cadaver database. These cadavers have been CT scanned and their anatomy was fully modeled in 3D before being imported into the platform. This yields the ability for users to study the anatomy of the entire body while understanding the differences of anatomical features in each person.
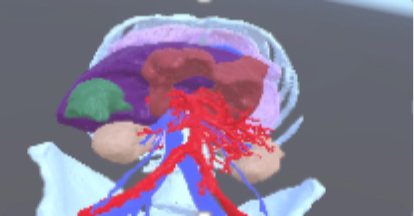
A fully modeled cadaver in virtual reality.
One of the focuses of the 3D modeling in the Visible Heart® laboratories is to enable virtual prototyping and deployment of medical devices within real human anatomy. Much can be learned about how a device is (or should be) designed by studying the device tissue interface. These virtual implantations can be studied within the virtual reality platform to gain insight about the device, its implantation position, and the device tissue interface within an immersive virtual environment.

Micra images.
Many of the cardiac specimens within the lab have devices already implanted in them. These specimens and their implanted devices can also be scanned, 3D modeled, and placed into the virtual reality platform. This unique opportunity allows the user to not only study the device tissue interface but reflect on the actual implant of the device and how it was truly deployed within the specimen.
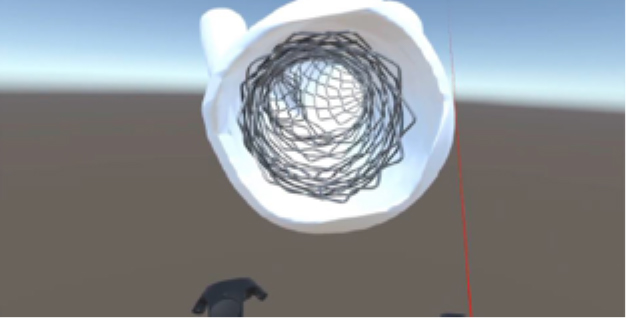
A bifurcation culotte stent in virtual reality.
The virtual reality platform contains a wide variety of features to enhance educational outcomes. These functions include the ability to change the scale of an anatomical model, the ability to hide or show the various models within a virtual environment, the ability to display the motion of a heart captured in a multi-phase CT scan, and many more. Additionally, the platform includes a custom anaglyph 3D output functionality to render the output display in 3D when using red/blue anaglyph 3D glasses. This allows one user to operate the virtual reality headset while a multitude of users can affordably experience the anatomical models in 3D.

Images of anaglyph functionality in virtual reality and being used by students wearing red/blue 3D glasses.
Devices
The Visible Heart Laboratories have established rich collaborations within the medical device community. Combining industry connections with our own anatomic library, we have generated computational models of medical device placements within human anatomy. These models help us to educate the community at-large about medical device therapy, while communicating the nuances of specific technologies with clinicians. Using 3D printing and virtual reality, we can fly through a stent in the left anterior descending coronary artery, follow a catheter through the femoral venous system, visualize a trans-septal puncture, appreciate the size of a leadless pacemaker, and much more.
Continue Reading
Cardiac Valves
Transcatheter aortic valve replacement (TAVR) devices are implanted and visualized within reanimated human hearts using Visible Heart® methodologies. These hearts are scanned using micro-computed tomography to obtain high-resolution images of the implanted TAVR frames. These scans are imported into a medical image processing system to develop computational models of the device. Subsequently, the computational reconstruction are 3D printed and developed as a virtual reality scene. A case study of an implanted CoreValve Evolut™ R and the 3D modeling process is shown in Figure 1.
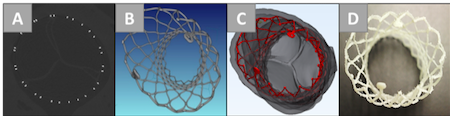
Figure 1: 3D modeling of a CoreValve Evolut™ R implantation within a reanimated human heart using Visible Heart® methodologies. The TAVR frame is visualized and analyzed through micro-CT scans (A), computational reconstructions (B,C), and 3D printing (D). (Adapted from Zhingre Sanchez, J. D.; Bateman, M.G.; Iaizzo, P.A. Multimodal imaging of a self-expanding transcatheter aortic valve replacement (TAVR) procedure in a reanimated human heart and post-implant analyses. The International Journal of Cardiovascular Imaging, November 2019, Volume 35, Issue 11, 2135-2137.
This 3D modeling process is important for studying the tissue-device interactions between the TAVR frame and real human aortic anatomy. The frame implant shape, evident through the imaging scans and 3D prints, can provide insight into strut deformations. The reconstructions detail how the device is positioned within the aortic root, which is important to analyze when minimizing paravalvular leakage and coronary obstruction. These analyses can educate both cardiologists about the implant process and medical device professionals with device design.
Education
Educational outreach is a cornerstone of the Visible Heart Laboratories' mission statement. Our mission includes teaching people from all walks of life—from middle school age to clinical cardiologists—about cardiac anatomy and device therapy. We host tours of the laboratory facility multiple times per week, and stage “A Heart to Learn” outreach events to bring the lab experience to groups who cannot make it to our facilities. 3D modeling plays a pivotal role in our educational outreach. We isolate and label interesting anatomy and devices in our models to aid our teaching. Additionally, we bring a 3D printer and virtual reality headset to each outreach session, to get the public excited about science. In this way, we aim to engage the future scientists of the world.
Artificial Intelligence
The Visible Heart® Laboratories are on the forefront of utilizing artificial intelligence to solve problems in the medical field. The focus thus far has been the development of pipelines that utilize convolutional neural networks to automatically segment anatomical features from CT and MRI scans and produce 3D models of said anatomy. These automatic segmentation pipelines produce a high-quality 3D model of an anatomic feature in a MRI/CT scan in mere minutes, whereas a human would require many hours to produce a 3D model of similar quality. This work yields the opportunity for large annotated anatomical datasets to be produced in a fraction of the time and workforce previously required. Pipelines such as these will likely see use in the future for reducing the time required to develop patient specific 3D anatomical models for surgical planning and post procedure scans for analysis.
Continue Reading

The four heart chambers segmented by an artificial intelligence pipeline (left) and a human segmenter (right).
The Visible Heart® Laboratories are also using AI in a variety of ways outside of automatic anatomical segmentation. Other current research topics include developing object detection networks to automatically detect and locate the position of anatomical features within a DICOM scan and using AI to perform point cloud registration between different anatomical models to quickly produce highly accurate statistical shape modeling of anatomical features within a dataset.