
Michael Tsai is ideally equipped to investigate a new frontier in heart disease risk and prevention
Nearly 20 million people worldwide die from heart disease every year, 700,000 of them Americans. A century ago, the American Heart Association (AHA) issued its first guidance document for physicians: “Nomenclature for Cardiac Diagnosis.” Neither the term cholesterol nor lipids appear in the document.
Today, the terms cholesterol and lipids are ever-present in any discussion of heart disease. Elevated low-density lipoprotein cholesterol (LDL-C) accounted for 4.5 million deaths in 2020, according to the AHA. In its 2018 “Guideline on the Management of Blood Cholesterol,” the American College of Cardiology (ACC) together with the AHA introduced a new lipoprotein risk factor to accompany elevated LDL-C. It is called lipoprotein(a) or Lp(a). An estimated one in four people has elevated Lp(a). “In the present document, an elevation of Lp(a) is considered to be a risk-enhancing factor [for atherosclerotic cardiovascular disease – ASCVD]. This is especially in those with higher Lp(a) values,” wrote the report’s authors. Lp(a) is now being described by some as “the final frontier in lipid management.” Successful lipid management can mean avoiding the main cause of death by disease.
LMP professor Michael Tsai, a biochemical geneticist, is one of the leading authorities in the world on the link between lipids, heart disease and heart failure.  In May, the American Association of Clinical Chemistry (AACC) honored Tsai with its AACC Academy Award for Outstanding Contributions to Clinical Chemistry in a Selected Area of Research. Awardees “have achieved national and international status for their pioneering efforts in an area of research considered fundamental to the science and have been considered among the world’s foremost experts in that specific discipline.” For Tsai, a long-time faculty investigator in LMP's Advanced Research and Diagnostics Laboratory (ARDL), the specific discipline is lipid biochemistry and genetics.
In May, the American Association of Clinical Chemistry (AACC) honored Tsai with its AACC Academy Award for Outstanding Contributions to Clinical Chemistry in a Selected Area of Research. Awardees “have achieved national and international status for their pioneering efforts in an area of research considered fundamental to the science and have been considered among the world’s foremost experts in that specific discipline.” For Tsai, a long-time faculty investigator in LMP's Advanced Research and Diagnostics Laboratory (ARDL), the specific discipline is lipid biochemistry and genetics.
An auspicious hunch
The key component of Lp(a) is apolipoprotein(a), or apo(a), which is thought to inhibit plasminogen, an important precursor molecule in dissolving blood clots. Tsai has had the Lp(a) molecule on his radar for three decades. A certain feature of the Lp(a) molecule – a version of a domain called kringle – caught his eye, specifically kringle 4 or K4. Kringle is named after the Danish pastry that is shaped something like a pretzel. The K4 units in apo(a) are highly homologous to the K4 units of plasminogen.
The number of apolipoprotein(a) K4 repeats in an individual, Tsai says, is determined genetically. The longer the K4 repeats in an individual’s apo(a) molecule, the lower that person’s blood serum Lp(a) level and potentially the lower the risk for developing ASCVD. The fewer K4 repeats – and African Americans “typically have a smaller number of kringle repeats” -- the higher the person’s Lp(a) level and associated risk – as much as four to five times higher risk. But could he demonstrate that elevated Lp(a) is a risk factor for atherosclerosis and coronary heart disease? And could he demonstrate it in diverse populations?
“Back then money was the limiting factor, the bottleneck,” Tsai said. He was able to carry out a limited amount of research in studying the K4 repeats, but he needed more funding. After many years, funding finally arrived and he could investigate his hunch.
The National Heart Lung and Blood Institute of the National Institutes of Health launched the Multi-Ethnic Study of Atherosclerosis (MESA) study in 2000. The study involves more than 6,000 men and women from six communities and their collaborating universities including the University of Minnesota. From the outset, Tsai headed up MESA’S central lipid lab services.  That gave him an opening. In 2011, he secured MESA funding to do a preliminary study on Lp(a) as a ASCVD risk factor. Three years later, Tsai and his colleagues reported an “association between lipoprotein(a) levels and coronary heart disease risk in different ethnic groups,” the first to do so. Four years after that, in 2018, the ACC and AHA task force issued its cholesterol management guideline that included elevated Lp(a) as a risk-enhancing factor for ASCVD.
That gave him an opening. In 2011, he secured MESA funding to do a preliminary study on Lp(a) as a ASCVD risk factor. Three years later, Tsai and his colleagues reported an “association between lipoprotein(a) levels and coronary heart disease risk in different ethnic groups,” the first to do so. Four years after that, in 2018, the ACC and AHA task force issued its cholesterol management guideline that included elevated Lp(a) as a risk-enhancing factor for ASCVD.
Since then, Tsai and his colleagues have shown that elevated Lp(a) puts people at greater risk for coronary artery disease and stroke, heart failure, the calcification of heart valves and vessels, heart arrhythmias, and hypertension or high blood pressure. Many of the findings are from the MESA study, but Tsai’s team is also pooling data from other large population studies including the Framingham Heart Study offspring cohort, ARIC (Atherosclerosis Risk in Communities), the Jackson Heart Study, and CARDIA (Coronary Artery Risk Development in Young Adults). These five observational population studies together involve more than 40,000 subjects from disparate ethnic and sociological backgrounds. Sophisticated biostatistics and data analysis are teasing out the contours of the “final frontier” in lipid management and risk profiles of different populations.
Surmounting intransigence with solutions
Exactly how Lp(a) undermines heart vessel and heart valve integrity isn’t understood, though its ability to induce inflammation is believed to be important. Only 13 percent of people at risk for heart disease and a mere 1 percent of the U.S population overall have been tested for their Lp(a) level. Despite its rising prominence as a heart disease risk factor, lipid testing panels in the U.S. do not – at least not yet -- include Lp(a) as they do in Canada, the United Kingdom, and the European Union. The Lp(a) blood test is accurate, reliable, and inexpensive, Tsai said, but cardiologists and general practice physicians in the U.S. are reluctant to recommend it. “No amount of scientific evidence seems to be enough to sway their opinion,” he said. In a commentary “Universal Testing for Lp(a): What Are We Waiting For?” a cardiologist put it bluntly: “Why are we not testing everyone for an extremely common and potent risk factor for the most lethal disease on the planet?”
It may be because there is no therapy for lowering Lp(a), like statin drugs for lowering LDL cholesterol. The only recourse for a high-risk patient is lipoprotein apheresis, the removal of Lp(a) from the bloodstream by a cell-separator machine every two weeks in the clinic. “Until treatment becomes available, physicians simply won't order the Lp(a) test even though it’s an inexpensive test, costing the lab less than $20 to do and should be covered by insurance,” Tsai said. Plus, it’s a “one-time test” because an individual’s Lp(a) blood level is genetically driven and not materially affected by diet, environmental factors, or aging, as is the case with LDL cholesterol.
Tsai is confident help is on the way for the estimated 60 million Americans with high Lp(a) and in particular for African Americans who Tsai and his MESA colleagues reported in 2015 have on average three-to-four times the Lp(a) level as other groups, helping to spur the launch of the African American Heart Study. Ionis Pharmaceuticals’ pelacarsen, which can lower Lp(a) dramatically, is in Phase lll clinical trials and should be up for FDA approval in two years, to be followed shortly thereafter by Amgen's olpasiran, also in Phase lll trials. Both drugs have shown the ability to lower Lp(a) 80-90 percent by inhibiting the molecule’s synthesis in the liver.
At least 14 companies are in the race to develop Lp(a)-lowering drugs employing a variety of technical strategies. Perhaps more than anything else, the race bears witness to Lp(a)’s rapid emergence in the field of lipids and cardiology and confirms Tsai’s hunch of three decades ago. Lp(a) is also coming into view as a public health concern, witness the commercial genetic testing firm 23andMe’s partnership with Novartis to raise awareness of Lp(a), “a little known genetic risk factor for cardiovascular disease,” as 23andMe put it in its announcement in March. 23andMe has more than 12 million customers worldwide. Novartis also collaborated with the Family Heart Foundation to create a national “Lp(a) Awareness Day” (March 24) and with the AHA in launching the “Lp(a) Discovery Project” that “will use an integrated, patient-centered approach to launch an Lp(a) screening measure and, using the Association’s current Integrated ASCVD Management Initiative infrastructure, track and test it nationally.”
Building bridges and coming full circle
Tsai’s journey to the forefront of lipid and Lp(a) research began when Laboratory Medicine and Pathology recruited him 1975 to set up a biochemical genetics laboratory. He recounts that experience, and his educational background, in his LMP “Legends in Pathology” video. His initial focus on improving the fetal lung maturity test took a turn in the mid-1980s when LMP professor Michael Steffes suggested that he join the Clinical Chemistry Division and branch out. “I said, okay, I’ll do lipids,” Tsai said. He had been doing lipid research both in developing a fetal lung maturation assay and phospholipid fatty acid profiling for several years, the latter after then-professor of surgery Frank Cerra asked him. Cerra’s intensive care patients tended to develop essential fatty acid deficiency after being hooked up to intravenous systems for protracted periods.
“From lipids, I became more interested in cardiovascular pathology,” Tsai said. He contacted Donald Hunninghake, who was head of preventive cardiology and the founder and director of the Lipid Research Laboratory, and they began a collaboration. “People asked me ‘What do you do?’ I’m a biochemical geneticist, I said. No, no, my research is in cardiology.” Tsai didn’t realize it at the time, but he was building a scientific bridge that joined biochemistry and genetics on one side with, on the other side, lipid and lipoprotein at the root of “the most lethal disease on the planet,” in the words of the cardiologist quoted above who called for universal Lp(a) testing.
In his early research on lipids and lipoprotein, Tsai investigated the molecular sizes and particle numbers of LDL and how triglyceride levels are inversely associated with LDL particle sizes. But Tsai’s major research foray into the world of heart disease was the biochemistry and genetics of homocysteine, a common circulating amino acid derived mainly from eating meat. “I started reading some papers on homocysteine, a risk factor for cardiovascular disease at high levels,” Tsai said. “This united my two disparate areas. It was a bridge. On the biochemical genetics side, my most important contribution was sequencing the homocysteine metabolizing enzyme-cystathionine beta synthase gene in the 1990s using the traditional Sanger DNA sequencing method, which is quite painstaking.”
Tsai returned to lipid biochemistry with his leadership in the MESA study beginning in the late 1990s. In the ensuing years he participated in several other population studies including CARDIA (Coronary Artery Risk Development in Young Adults), GOLDN (Genetics of Lipid Lowering Drugs and Diet Network), the Physicians’ Health Study, and the Women’s Health Initiative, among others.
After building a bridge between biochemical genetics and lipids/lipoprotein in heart disease, Tsai came full circle. Some two decades after concluding his homocysteine research he returned to it with the MESA study “Association between homocysteine and vascular calcification” published in 2020, suggesting homocysteine may be a biomarker “in predicting risk for incidence and progression of vascular calcification.” Tsai’s laboratory is currently exploring how high levels of homocysteine, Lp(a), and C-reactive protein (CRP), an indicator of inflammation, may work in tandem to put people at even greater risk for coronary artery disease and stroke.
Sixty-five years ago University physiologist and professor of public health Ancel Keys launched his Seven Countries Study “to investigate diet and lifestyle along with other risk factors for cardiovascular disease.” 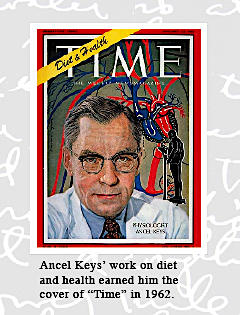 As I wrote in my piece “Meet Monsieur Cholesterol,” published in 1979, Keys “traced cholesterol buildup to saturated fats -- fat molecules with a full load of hydrogen atoms -- found mainly in meat and dairy products.” Keys and his wife Margaret championed the now-popular Mediterranean diet in their 1959 book Eat Well and Stay Well.
As I wrote in my piece “Meet Monsieur Cholesterol,” published in 1979, Keys “traced cholesterol buildup to saturated fats -- fat molecules with a full load of hydrogen atoms -- found mainly in meat and dairy products.” Keys and his wife Margaret championed the now-popular Mediterranean diet in their 1959 book Eat Well and Stay Well.
Tsai has been investigating the dietary effects of polyunsaturated fatty acids (PUFAs) for years. Currently, his team is exploring the potential benefits of omega 3 and omega 6 fatty acids in the context of many disease states: chronic kidney disease, type 2 diabetes, heart failure, lung disease, aortic valve calcification and stenosis, heart arrhythmias, microvascular diseases such as diabetic retinopathy, and age-related macular degeneration, among others. His laboratory is where genetics, biochemistry, diet, lifestyle, and reproductive health converge at the molecular level.
Again, coming full circle. This line of inquiry returns Tsai to the arena where he got his start in LMP: Fetal and newborn health. With support from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), Tsai’s team has explored the association of PUFAs with fetal growth, neonatal anthropometry as a measure of newborn health, gestational diabetes, and other conditions associated with pregnancy and birth. Last December, NICHD awarded Tsai a 10-year research contract of up to $49 million for his laboratory to serve as the central biomedical assay laboratory for the NICHD Division of Population Health Research (DiPHR). The Division advances health and disease outcomes in populations “by focusing on successful reproduction, the health and well-being of pregnant women and their infants, and the optimal growth and development of children and adolescents across the lifespan.”
From his birth in Shanghai, his early education in Hong Kong, his undergraduate and advanced degrees from Wisconsin to the University of Minnesota where he has spent his career, Tsai’s life has been marked by an extraordinary passion for discovery and for resisting rigid scientific boundaries that can limit discovery that changes people’s lives for the better. Tsai’s professional life has also been marked by the invaluable trait of stamina. Which means that we can count on him to continue his drive to push back the frontiers of what we don’t know.



