Applying noninvasive stimulation to help TBI patients overcome mental fatigue
Functional neurosurgeon and neuroscientist David Darrow, MD, MPH, of the Neurosurgery Department, works collaboratively on research with several U of M departments and with other institutions. In a new collaboration, he and a research team, co-led by psychiatrist and neuroscientist Alexander Herman, MD, PhD, of the Psychiatry and Behavioral Sciences Department, are working with the Uniformed Services University (USU) of the Health Sciences in Bethesda, MD.
This unique partnership with the U’s Medical School, Minnesota’s Medical Alley, and Fairview, has USU funding 13 research studies at the University to address civilian and military service health issues. The primary focus is on traumatic brain injury (TBI).

Darrow’s team applied for and was awarded one of the USU grants and will use the three years of funding to address a common issue that comes with TBI – mental fatigue. Their study is titled, “Circuit-based Neuromodulation to Improve Mental Fatigue After Traumatic Brain Injury.” In addition to colleagues at USU and researchers in their lab, Darrow (pictured here) and Herman are working with Alexander Opitz, PhD, U of M Biomedical Engineering (focus: computational modeling), and Tom Bergman, MD, at Hennepin Healthcare in Minneapolis. Nurse practitioner Tara Nash, RN, FNP-BC, runs the study from Hennepin Healthcare in her role as Restorative Neurotrauma Lab manager.
Passion for neuromodulation
Darrow brings his passion for neuromodulation to this project. He is amassing extensive experience with both invasive and noninvasive stimulation, using it to treat spinal cord injury and conditions such as movement disorders and epilepsy. Herman is exploring the use of neurostimulation to treat psychiatric conditions such as depression. They want to jointly apply their expertise to help brain-injured Veterans and civilians overcome their mental fatigue.
“Many patients have post-TBI fatigue – they feel tired and don’t want to get up to do things because the world seems disproportionately hard,” said Darrow. “For this project, we’re pairing tools from neuroeconomics1 – which can quantify how difficult you perceive the world to be – and a new type of neuromodulation that we validated specifically for the TBI population at Hennepin Healthcare.”
Mental fatigue and depression
If the symptoms related to mental fatigue sound familiar, that shouldn’t be a surprise. They are like those associated with depression.

The Herman Darrow Lab is focused on redefining clinical expression or phenotypes of depression based on the brain circuits involved. “We believe many things are related to depression, anxiety, or addiction,” said Herman (pictured here). “These conditions involve overlapping circuits in the brain and one of the more important ones is associated with the motivation to apply cognitive effort, which underlies mental fatigue.”
Cognitively difficult tasks
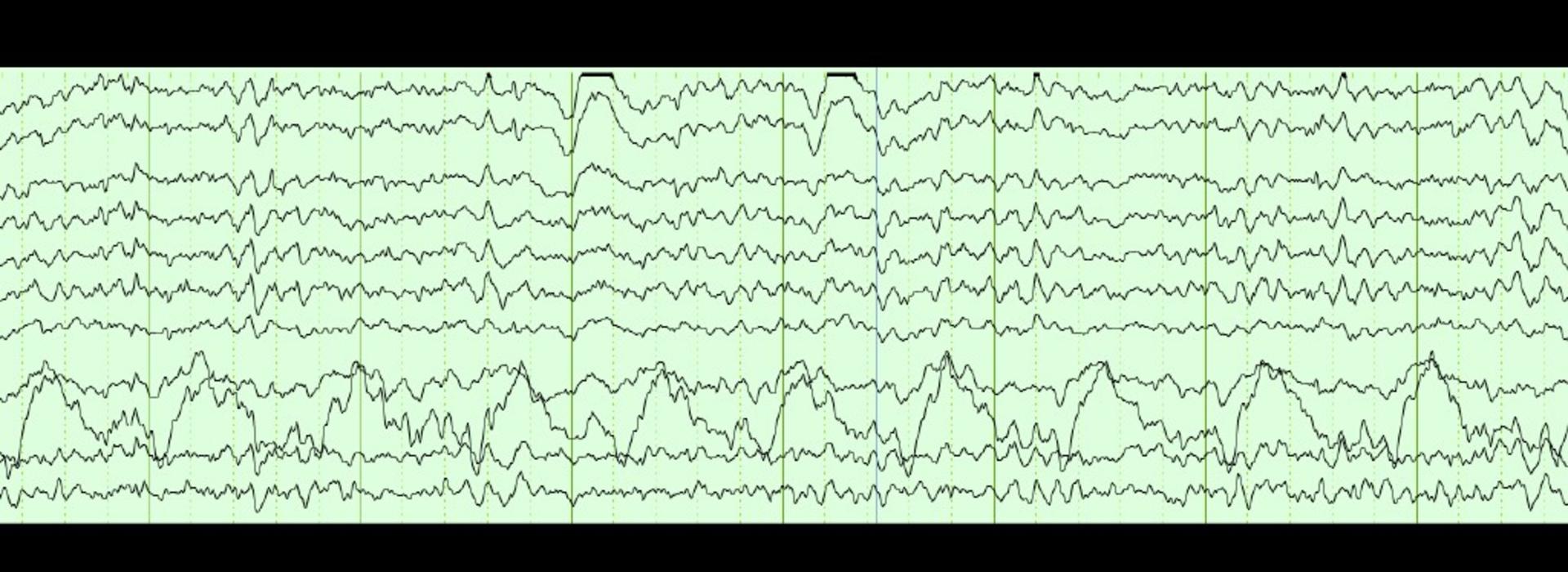
The team’s goal is to show that noninvasive transcranial alternating current stimulation (tACS) makes the world seem easier to navigate and helps entrain the brain to perform cognitively difficult tasks, which are markers for being able to tackle the world at large, according to Darrow. “The interesting thing about tACS is that we’re wiggling electricity on the scalp back and forth in the beta band between 13 and 30 hertz,” he said. “It’s one of the higher frequencies in the brain that is often involved in cognitively difficult tasks.”
Darrow and Herman chose the circuits they’re targeting with tACS because they know that trauma preferentially hits broad, long circuits because of the brain’s movement during the event. “No matter how you hit your head, the rotational and shear forces that are produced contribute to the same pattern of damage,” said Darrow. “There is so much variability associated with TBI – that’s why it’s hard to define exactly which circuits in the brain are affected.” The impact on these circuits isn’t always apparent at first glance, he added.
Two protocols
That’s why the research team will start the stimulation six weeks after the injury, following measurements taken during the inpatient stage. They will enroll 24 people who will receive both sham and active stimulation. After the team gets everything set up during the first year of the study, they will take enrollees through two protocols. “One is to monitor them as inpatients performing computerized cognitive tasks,” said Darrow. “That will help us quantitatively assess their cognitive effort and how they perceive the world.” The second protocol brings participants to the lab twice a week for two weeks for a couple of hours. During each session, they receive either sham or active stimulation and then they will cross over to receive the other.
“tACS was specifically developed to entrain oscillations,” explained Herman. “Optimally, brain circuits work at specific frequencies. In TBI, every time you want to get to that optimal state, some percent of the fibers aren’t working normally. You can’t stay in that optimal state because you get distracted or feel tired. What tACS does is hold you at the optimal frequency so the oscillations can facilitate what you want to do. It will help these patients work their way out of the issues that plague them.”
Multiple applications
Although the team is just looking at TBI for this study, the work they’re doing could apply to mental fatigue in other populations, such as those with dementia, chronic fatigue syndrome, and long COVID, according to Nash. “We also hope to help reduce the medications people have to take, enabling them to function as they want to,” she said.
1According to the Society for NeuroEconomics, neuroeconomics is a field that represents the confluence of economics, psychology, and neuroscience in the study of human decision making.



