
Chou Lecturer notes that neurosurgeons are at the forefront of diagnosing and treating pituitary conditions
On June 22, Nelson Oyesiku, MD, PhD, FACS, gave the endowed Shelley N. Chou Lecture at the University of Minnesota Campus Club in Minneapolis. His presentation was titled, “Evolution and Revolution in Pituitary Medicine and Surgery.”
Oyesiku is Professor and Chair of the Department of Neurological Surgery, and Professor of Medicine (Endocrinology) at the University of North Carolina, Chapel Hill. He has developed one of the largest practices in the country entirely devoted to the care of patients with pituitary tumors and has performed more than 4,000 pituitary tumor operations.

Broadly speaking, these tumors are divided into two types: nonfunctional and functional. “That’s based on whether or not the tumor produces a hormone in excess,” explained Oyesiku (pictured here). “Some produce an excess of adrenocorticotropic hormone, causing Cushing’s syndrome; some produce too much growth hormone, causing acromegaly, or too much prolactin causing hyperprolactinemia.” On the other hand, nonfunctional tumors can cause a deficit in hormonal secretion, he added.
During the lecture, Oyesiku traced the long history of pituitary surgical techniques, focusing on the endonasal approach that helped surgeons address tumors in this area more safely. “We talked about technical innovations that brought the operative field into better view through instruments such as the endoscope and microscope,” he said. “Our knowledge of the human physiology behind how the pituitary hormonal system functions and discoveries of medications such as dopamine agonists, somatostatin analogs, and receptor antagonists have also shaped the treatment of pituitary tumors related to hormonal conditions.”
When Oyesiku thinks about revolutionary treatments or surgical techniques in pituitary medicine that have emerged over the years, endoscopy tops his list. “It was one of the first tools that enhanced our ability to visualize and remove pituitary tumors,” he said. “This has been key to our ability to treat these tumors surgically with little or no cosmetic disfigurement and little or no disruption of vital anatomy,” said Oyesiku. “Using the nasal passage as a natural corridor provided a minimally invasive access route that results in maximal effectiveness.”
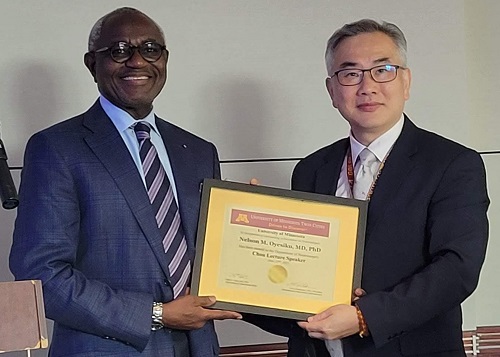
Oyesiku (pictured here with Department Head Clark C. Chen, MD, PhD) also noted the importance of how physicians have come to understand the key relationship between pituitary hormone function and clinical symptoms. “We now know the mutations and cellular changes that cause pituitary dysfunction,” he said. “That has helped us understand how to better treat pituitary tumors and has provided adjuncts and alternatives to surgically removing some of them.”
It's no surprise that not all questions about treating pituitary conditions medically or surgically have been answered. “We still need further information and discovery about what causes many of these tumors,” said Oyesiku. “In patients with Cushing’s syndrome or acromegaly, we understand what’s responsible in only about 40 to 50 percent of the cases. We also do not have satisfactory information about what causes other pituitary tumors.”
Oyesiku, however, is hopeful about the future of pituitary medicine. “We are getting better at understanding and visualizing what’s going on inside the cellular structure of these tumors,” he said. “With the advent of molecular biological techniques, for example, we can dissect inside the cellular mechanisms responsible for tumorigenesis. We are also excited about innovations to come in drug discovery.”



