Neuroscience Unit nursing team celebrates an amazing accomplishment – no falls with injury for a year
According to the Agency for Healthcare Research and Quality, “each year, somewhere between 700,000 and 1,000,000 people in the United States fall in the hospital. A fall may result in fractures, lacerations, or internal bleeding, leading to increased health care utilization. Research shows that close to one-third of falls can be prevented.”
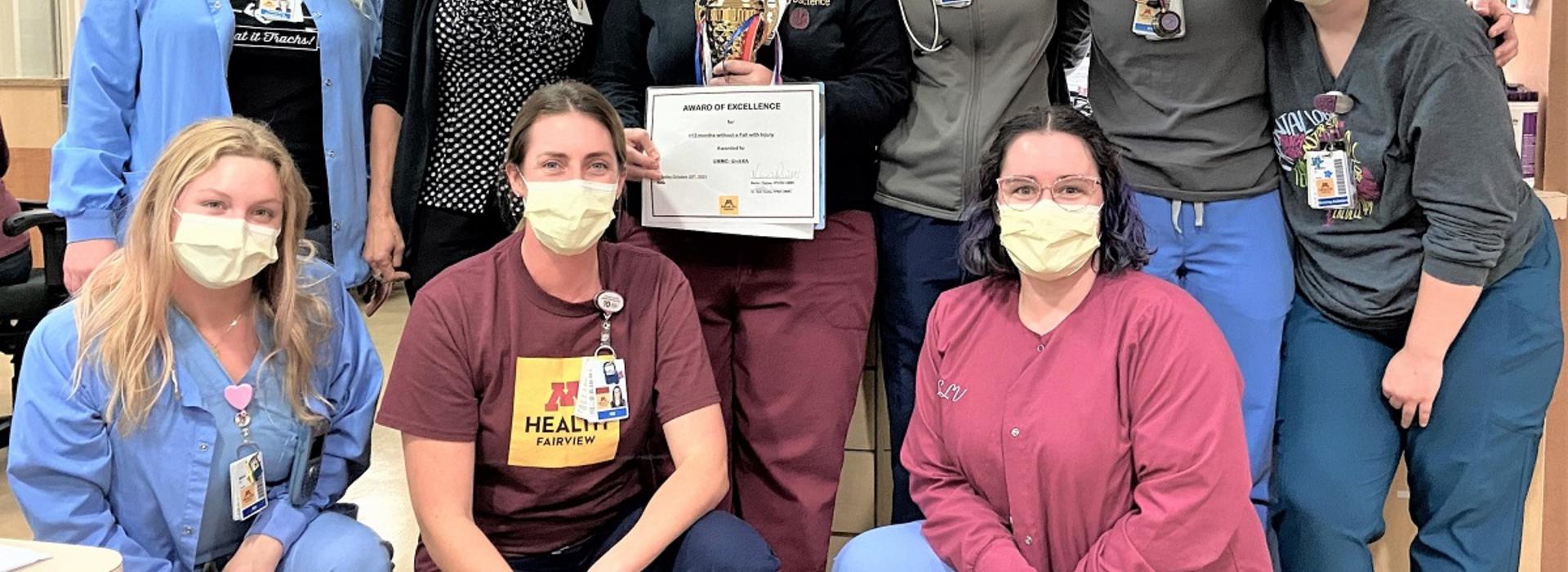
The nursing team on the Neuroscience Unit (6A) at the University of Minnesota Medical Center (UMMC) recently crossed a significant threshold regarding patient falls. On October 25, 2021, they celebrated a year of having no falls with injuries.
Challenging patient population

To understand the significance of this achievement is to understand the patient population being served by this team. It can include patients with epilepsy or with significant cognitive impairment. “We also have patients with head, neck, and spine issues as well as those who have had laryngectomies and tracheostomies,” explained Philip Wills, RN, BSN (pictured here with Brittany Fjeld, NST). “There can be a lot of cords attached to the patients and equipment around their beds.”
The Unit’s patients often go through post-operative delirium and even when that settles down, there may be a new norm for their cognition. “The confusion that patients experience following their surgery can last throughout their hospital stay,” said Wills. “As they become more physically able-bodied, they still may not clear their cognitive hurdles as quickly. That combination increases the risk for a fall.”
Use of sensitive alarms
Some of the steps the team has taken to prevent falls include the use of Zone 2 bed alarms and Zone 2 magnets on doors to warn everyone that the patient is at risk for a fall. “Zone 2 relates to the sensitivity of the alarm,” explained Fjeld. “It describes how far you want the patient to move before an alarm sounds. The Zone 2 alarm goes off before the patient is fully out of bed. It gives us more time to respond to prevent a fall.”
And respond they do. Physicians and visitors to the floor are often surprised by nursing staff sprinting down the hallway to get to a bed alarm. “They witness our urgency,” said Wills. “A lot of stuff can be considered important during training or when you’re floating on our staff but when you see it take place, you can understand the priority we place on preventing falls.”
Trained from the beginning
Training is key to fall prevention on 6A. “From the beginning, we train all of our new staff on the importance of responding to bed alarms and preventing falls,” said Fjeld. “We also talk about preventing falls in huddle every day, which helps keep it fresh for everyone.”
When patients are discharged, the team ensures that fall prevention continues to be important. “We set the new baseline at the hospital – what the new routine will be for the patient’s mobility,” said Wills. “We hope that what we do in the hospital to prevent falls will transfer to the home or acute rehab setting.”
Education is crucial
Education about that transition is crucial. “When patients are going home, we tell them about the same mechanisms we use at the hospital – to stay within arm’s reach of a person, bed, couch, chair or table, to encourage the use of walkers or canes, and to always have shoes on,” said Fjeld.
Accomplishing this took an amazing amount of teamwork on the Unit. “It’s part of our culture,” said Fjeld. “It’s ingrained in everyone’s mind — we know we have a system about what to do to keep our patients and ourselves safe. We are all on the same page about it – there isn’t any miscommunication that can cause unwanted falls.”
Multidisciplinary effort
“We have to give a shout out to our physical and occupational therapists because they help increase our patients’ mobility, which is the ultimate goal, while keeping them safe from falls,” added Wills. “They use the same bed alarm system that we’re so excited about.”
According to Jenna Doyle, RN, BSN, SCRN, 6A Patient Care Supervisor, about 40 to 50 bed alarms go off every eight-hour shift on the Unit. “Our nursing staff immediately stop what they’re doing to go make sure our patients are safe,” she said. “The credit for having no falls with injury for an entire year goes to them and the culture they helped create.”
“I am incredibly proud of the 6A nursing team,” said neurosurgeon Andrew Grande, MD. “They set a goal to reduce falls with injury a year ago and worked very hard to achieve that goal. Most importantly, they changed the culture around falls, and it has been extremely effective. In the end, the efforts they make on a daily basis have improved the care of our patients.”
Key words:
#fallprevention
#patientsafety
#NeuroscienceUnit
#nursingteam
#culture
#training



