Child and Adolescent Psychiatry Fellowship making meaningful changes to improve the fellows’ experience

What is it that major league baseball teams often say? “We’re in a rebuilding year.” Child and Adolescent Psychiatry (CAP) Fellowship Program Director and Assistant Professor Jacquetta Blacker (pictured here), MD, MA, can relate.
Earlier this year, Blacker took over the reins of the department’s two-year CAP fellowship, which needed some rebuilding. “We wanted to create an organizational structure that better supported the fellows’ educational activities and our faculty’s ability to work with the fellows effectively,” she said.
Ready for graduation
Blacker is leading a rebuilding team that includes Assistant CAP Fellowship Program Director Aimee Murray, PsyD, LP, who “is helping guide the processes and bringing her psychology perspective to make sure we didn’t miss anything.” Working with others in the Child and Adolescent Mental Health Division, the team is creating a clearer, more coherent didactic schedule with curriculum that covers material a child psychiatrist needs to know to be ready for graduation. “We want them to be capable, safe, competent clinicians, and to be well prepared for their board exams,” Blacker said.
Improving communication and feedback has been a key priority during the rebuilding process. “Fellows needed a more effective way to communicate good things and bad things about the program so that positive implementations could be fostered and grown,” said Blacker. “They also needed a structured, regular way of getting feedback from faculty about their own performance.”

Constant feedback
The rebuilding team is emphasizing constant feedback rather than the high-stakes feedback provided during the semi-annual evaluation, according to Professor Phil Luber (pictured here), MD, Director for Psychiatry Education, who worked with the team for several months. “We wanted more formative feedback to help the people and program improve,” he said. “Part of that is changing the culture to accept feedback, which will help improve fellow and faculty performance and faculty supervision.”
Evaluations are short with an emphasis on meaningful narrative, Luber continued. “They’re designed to quickly capture what the fellows and faculty are doing well, and providing two specific areas of improvement,” he said. “There is also an interactive piece during which faculty and fellows give each other feedback. We presented this process during the national meeting of the American Association of Directors of Psychiatric Residency and received a lot of good feedback about it. It makes it so everyone can improve in an environment where there is constant, useful feedback – short, sweet, timely, and to the point.”
Quick, easy, timely
To enable one level of feedback, the team is creating quick, easy-to-complete electronic surveys that fellows will turn in after a didactic session or a rotation. “We will then distill the information at the program leadership level and send feedback to the people involved,” said Blacker. One of the refinements the team is considering includes providing a QR code that fellows can scan to provide any kind of feedback. “We’ll see how it works,” she noted.
The rebuilding team is also using the skills and talents of the Child and Adolescent Mental Health Division faculty to help improve the fellowship. “We asked people to do what they are good at,” said Blacker. “We got different people to participate more and rewarded them in different ways. We started giving monthly Meaningful Difference Awards to faculty that the fellows felt made a big difference to their learning.”

More well-rounded experience
Second-year fellow, Tom Briese (pictured here), MD, noticed the changes. “The program has done a nice job of revamping the didactic series schedule to highlight faculty who are well-versed in their fields, whether that was psychotherapy, pharmacology, neurology, or neuroscience,” he said. “The time for didactics was also extended, going from three hours a week to four. Both those changes led to a more well-rounded educational experience.”
The team also had to redesign the fellowship’s outpatient clinic experience. Faculty members Gail Bernstein, MD, and Jonathan Homans, MD, took on that challenge. “Many changes were made,” said Briese. “When I started the fellowship, we were doing half days in the clinic per week. That felt like we weren’t going to see enough patients to meet ACGME [Accreditation Council for Graduate Medical Education] requirements. Expanding to a full day in clinic, we’ve been able to help more patients and give better access to care while incorporating a roundtable discussion during which we come together and talk about challenging patients.” It also enabled the fellows to maintain a panel of continuity patients, which they see over time – another important ACGME requirement, according to Blacker.
Hats off to leaders
She gives kudos to Department head Sophia Vinogradov, MD, and Child and Adolescent Mental Health Division Head Katie Cullen, MD. “They gave us any resources we needed – it couldn’t have been done without them,” said Blacker. “We also had fantastic fellows who worked hard to give us feedback and try new things. It was a team effort.”
And when ACGME announced they wanted to do a site visit two weeks after she accepted her new role as CAP fellowship Program Coordinator, Emma Fisher went into action. “She was so organized and efficient and made all the massive amounts of documentation come together seamlessly,” said Blacker. “She’s amazing.”
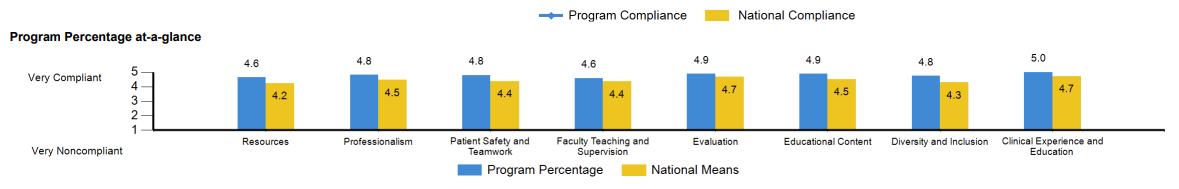
The results of the audit were also amazing. Across the board, the fellows scored the fellowship better than the national means for similar programs (see below). “It suggested that there had been a genuine improvement in the quality of the fellows’ lives,” said Blacker. “They were happier and enjoying the training experience more. It’s two years of their lives; it’s important for them to have some fun even though they’re working hard and learning.”
Clinically competent, academically active
Ultimately, Blacker and the fellowship team want their fellows to become clinically competent and develop a reputation regionally for being so. “I want people to say, ‘Oh, it’s a U of M fellow, they must be good,’” she said. “That will come from clinical exposure to a variety of cases and how to manage them, ways of thinking analytically about diagnosis and treatment options, and then communicating that well with patients and their families. On the academic side, I want them to become increasingly familiar and comfortable with not just consuming scientific literature but contributing to it. I want them to be academically active in the community so they’re producing case reports and scholarly work and teaching themselves. The fellows are keen on us moving in that direction.”
Perhaps the best testimonial is that given by a fellow. When asked if he would recommend the fellowship to others, Briese said, “Absolutely. I’m confident in the core faculty we have. Dr. Blacker is a phenomenal program director and an outstanding educator. It feels like she’s constantly getting feedback from us and we’re more than happy to give it. And she incorporates it. Things change rapidly in a way that frankly none of us are used to seeing. To have a program that’s that responsive to the needs of the fellows, you can’t ask for anything more.”