Residency
Welcome to the Adult Psychiatry Residency Program at the University of Minnesota! We aim to create psychiatric experts and leaders for the state of Minnesota and beyond.
Program Leadership

Karen "Kay" Powell, DO
Program Director
powel784@umn.edu

Jeremy Bydlon
Program Administrator
respsych@umn.edu
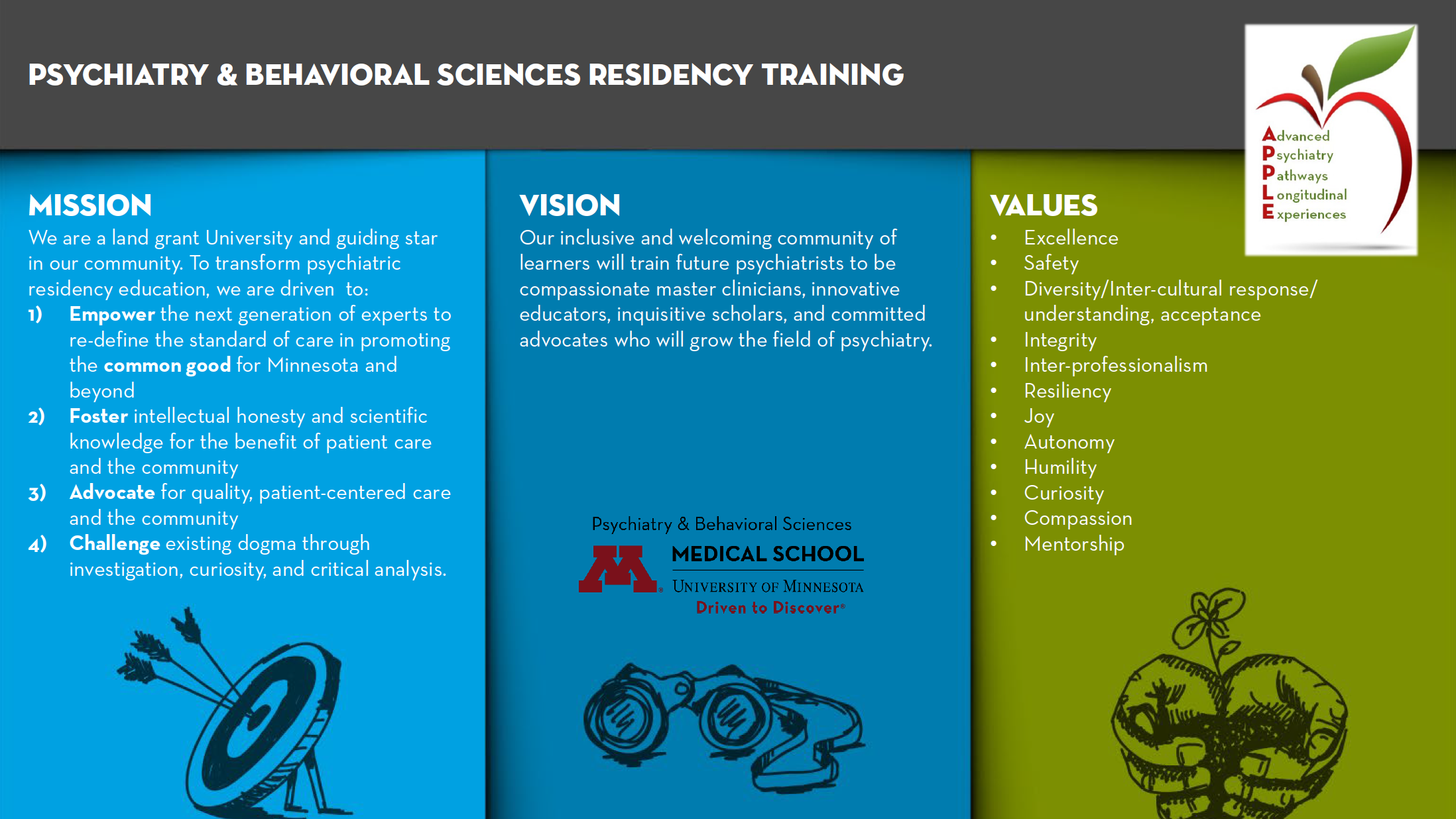
Vision and Values
We support our residents to become talented clinicians prepared to serve individuals who have mental health needs with sensitivity, compassion, and rigorous excellence. More importantly, we encourage our residents to grow as team leaders and team members, as optimal mental health care always occurs in a team context.
As a resident, you have many opportunities to study with highly knowledgeable faculty who are dedicated to excellence in patient care and scholarship. Many of our faculty are recognized as national and international experts in their fields. We have special strengths in treatment-resistant depression, stress and trauma, early childhood development, adolescent mood disorders, psychosis spectrum illness (including first episode of psychosis), and addictions. We also have a number of excellent training opportunities in women’s mental health, forensic psychiatry, veterans’ mental health care, community psychiatry, and services for marginalized communities.
Inclusive Excellence
Our department is strongly committed to the journey of eradicating racism and fostering inclusive excellence. For our department’s position statement, please see the Antiracism Statement on the dropdown below and consider this video.
Psychiatrists should represent multiple backgrounds, life experiences, and viewpoints to best serve our patients and advance the field. We are eager to appreciate the unique strengths and contributions of each individual, and we are mindful of every applicant’s complex background including racial, ethnic, sexual, and gender identity, as well as socioeconomic status and geography. A diverse group of residents strengthens our program, enhances our delivery of patient care, and fosters change to reduce healthcare disparities.
We have many active DEI initiatives in the Department and we encourage everyone to participate (more information here). As a resident, you can partner with the program’s Diversity and Inclusion (D&I) Thread Lead, a resident who is ready to support residents from diverse backgrounds, to develop curricular and outreach projects, and to represent the residency program at the Department D&I Committee. For more information, please contact our current D&I Thread Lead Jonas Attilus at attil002@umn.edu.
You may also contact our current residents with any additional questions about the residency experiences (see the sidebar on that page).
Additional resources for medical students and prospective residents:
- 5 keys to navigating the residency Match as an LGBTQ applicant – American Medical Association
- Key tips for medical residents facing microaggressions – American Medical Association
- Racism and Medical Education: Telling the Full Story – American Association of Medical Colleges
Anti-Racism, Discrimination and Oppression Statement
The Department of Psychiatry & Behavioral Sciences condemns racism, discrimination, and oppression in all forms. We affirm that racism and oppression are public health crises with serious mental health consequences for the communities we serve. We commit to listen to and promote Black, Indigenous and people of color. We also commit to amplify their calls for change. We have work to do. We are part of a system that has allowed racial disparities in medical outcomes.
Our work is guided by the following principles:
- Amplify the voices of those most directly affected by racism and oppression to restore justice. Racism and oppression are not their responsibility to solve; the responsibility to dismantle racism falls on those who have benefited from it.
- Ensure a just, equitable, and inclusive educational, clinical, and research environment.
- Take all needed steps to identify and dismantle unjust and inequitable systems, as individuals and collectively. This includes systems within our medical school, our university, and society at large.
Salary and Benefits
- Vacation
- 15 days per year (PGY1 and 2)
- 20 days per year (PGY3 and 4)
- Sick Days: 10 days per year
- Conference Days: 5 days per year (can be used for Step/COMLEX/Board prep)
- Salary (UMN GME 2022-2023)
- PGY1 $68,531
- PGY2 $70,640
- PGY3 $73,038
- PGY4 $75,734
- Conference Travel Fund: up to $1000 in grant support for academic conference participation (travel, registration fees, lodging, and/or transportation) for residents presenting at local, regional, or national conferences.
- Book Fund
- PGY1-4: $350 per year
- Additional $100 per year for poster printing
- White coats provided with free dry cleaning at the VA
- Meal cards provided for inpatient rotations
- UMMC ($900/year)
- VAMC ($75/month)
- Parking is free at both the UMMC and VAMC
- Medical, dental, disability and life insurance are offered thought the University of Minnesota GME Office in addition to optional flexible spending accounts and voluntary retirement options. For more information on UMN GME benefits please go to: https://shb.umn.edu/health-plans/rfi
Riverside Campus I/O Clinical Sites

The academic psychiatry inpatient teams and adult outpatient clinics are located at the University of Minnesota Medical Center (UMMC) Riverside Campus. Residents also rotate through specialized services here such as ECT and addictions treatment.
Masonic Children's Hospital

The M Health Fairview UMMC Masonic Children's Hospital hosts the Pediatrics rotation during the intern year. This is also the site of the Adolescent Dual Diagnosis (Mental Illness and Chemical Dependency) inpatient unit.
VA Medical Center

Interns rotate on the VAMC’s inpatient psychiatry unit and on the Internal Medicine Hospitalist team. They also complete their Neurology requirement at the VA. After internship year, residents return to the VA for electives in Geropsychiatry and Consult/Liaison in PGY2. They also complete 24-hour call shifts at the VA their second year. Multiple elective opportunities are offered at the VA for PGY3 and PGY4 residents (see “Electives”).
ARTC and St. Peter State Hospital
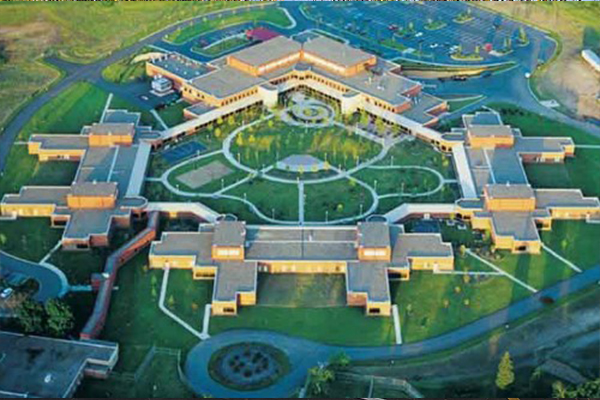
Residents complete their Forensic Psychiatry rotation at the Anoka Regional Treatment Center (ARTC) and St. Peter State Hospital, as well as through the Hennepin County Court System. The ARTC is a 200-bed psychiatric hospital located in Anoka, Minnesota (approximately 45 minutes north of the Twin Cities), for patients with severe mental illness. Located near Mankato, Minnesota (approximately 75 minutes west of the Twin Cities), the St. Peter State Hospital is a 360-bed hospital for patients with severe mental illness and/or patients deemed to be extremely dangerous.
Coordinated Specialty Care in Early Psychosis

Two nationally recognized clinical sites – one at our Riverside Clinic and one at our Saint Louis Park location (pictured) – provide specialized coordinated care for individuals in the early phases of psychosis spectrum illness. These clinics implement a recovery model and are part of a national network – the Early Psychosis Intervention Network (EPINET) – that is actively engaged in measurement-based care and practice-based research. Residents become part of our interprofessional teams during their PGY 3 and/or PGY 4 years and aid young individuals in recovering from initial episodes of psychosis.
Community Psychiatry Sites

Residents have the opportunity to rotate through various clinics and services for community, public, and integrative psychiatry exposure.
The Community University Health Care Center (CUHCC — pictured) is a federally qualified health care center specializing in integrative primary care that largely serves the Hmong, Somali, and Native American populations of Hennepin County. The clinic offers medical, dental, mental health, advocacy, legal, and other programs. Further integrative care opportunities are available through the Fairview Integrated Primary Care Clinic on the UMMC Riverside Campus or various Fairview Primary Care clinics (e.g., Smiley’s Family Medicine Clinic).
Residents who would like exposure to Assertive Community Treatment (ACT) services have the opportunity to rotate with Guild Assertive Treatment Services based in St. Paul, Minnesota. Exposure to private mental health care systems such as Prairie Care and Canvas Health is also available.
Faculty and Staff

Karen "Kay" Powell, DO
Program Director
powel784@umn.edu

Matej Bajzer, MD, PhD
Associate Program Director
mbajzer@umn.edu

Tolu Odebunmi, MBBS, MPH
Associate Program Director (Curriculum, Didactics, and Resident mentorship)
odebu001@umn.edu

Melvina Bissonette, MD
Associate Program Director, Minnesota VA site
melvina.bissonette@va.gov

Felicia Hansell, MD
Associate Program Director
hans4864@umn.edu

Lionel Wininger, PhD, LP
Assistant Program Director
winin006@umn.edu

Richelle Moen, PhD
Assistant Program Director
moenx008@umn.edu

Jeremy Bydlon
Psychiatry Residency Program Director
respsych@umn.edu