Unique U of M study looking at impact of using ketamine for treating Veterans with comorbid PTSD and MDD
In a National Institutes of Health-funded study that is the first of its kind in the United States, Principal Investigator C. Sophia Albott, MD, MA, and her research team are exploring the impact of using repeated ketamine infusions to treat U.S. Veterans who have been diagnosed with both PTSD (post-traumatic stress disorder) and major depressive disorder (MDD). “When we see people who develop problems because of trauma exposure and their symptoms start to get worse, it isn’t just PTSD that we see,” said Albott. “They often have comorbid conditions such as MDD.”
There aren’t many treatment options other than psychotherapy for PTSD, according to Albott. “It’s the gold standard,” she said. “A few medications can help with symptoms, but not many. There are more treatment options for MDD; however, there is nothing available for co-morbid PTSD and MDD.”
Understanding recovery

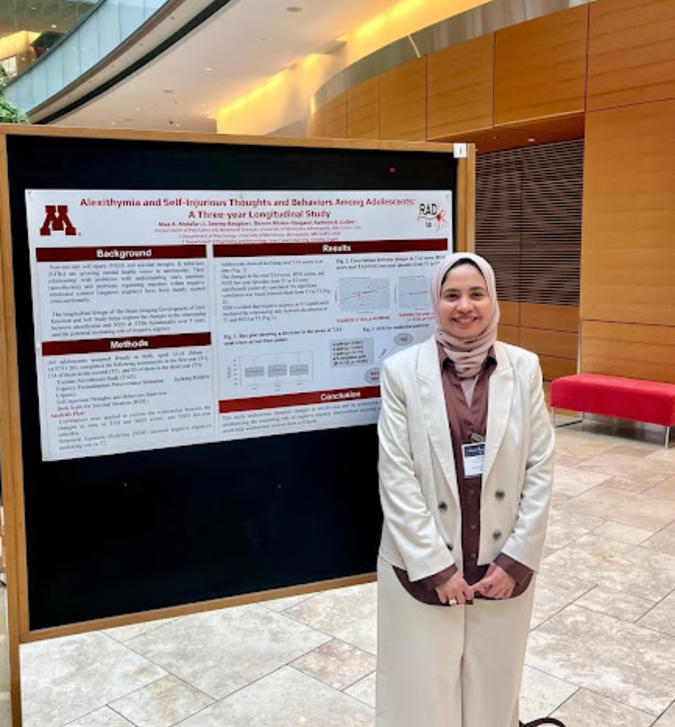
Other ketamine trials have looked at each condition separately but not together. “What we hope to come away with is a good understanding of what recovery from PTSD and MDD looks like as a result of the repeated ketamine infusions,” said Albott (pictured here), who is Head of the Division of Adult Mental Health for the U’s Psychiatry and Behavioral Sciences Department. “We have pilot data that shows giving a short course of multiple infusions is effective for treating these comorbid conditions.”
Another novel aspect of the study is that pre- and post-neuroimaging will be done to characterize the brain networks that underlie any recovery that the research team sees, according to Albott, who is being mentored on the imaging portion of the project by Associate Professor Katie Cullen, MD, of the Department of Psychiatry and Behavioral Sciences, and for statistical analyses by Paul Thuras, PhD, Adjunct Faculty for the Department of Psychiatry and Behavioral Sciences and Statistician at the Minneapolis VA Medical Center. Her primary grant mentor is Kelvin Lim, MD, Professor in the Psychiatry and Behavioral Sciences Department.
Why use ketamine?
Ketamine was developed in Belgium in the 1960s as an anesthesia for animals, and in 1970, was approved by the FDA for use in humans as an anesthetic. More recently, the drug has been involved in studies like Albott’s as a potential treatment for mental health conditions such as depression.
A group of Yale researchers laid the groundwork in the 1990s during a study in which they treated people with MDD by giving them a sub-anesthetic infusion of ketamine, according to Albott. Although numerous hypotheses have been suggested for how ketamine exerts its clinical benefit, studies showed that the drug may produce its antidepressant effects by triggering the release of glutamate, which then stimulated growth of new synapses between brain cells. “This resulted in a rapid improvement in depression symptoms with a peak response 24 hours after the infusion,” said Albott.
Remarkable effect
She believes that’s remarkable for a couple of reasons. “First, it creates a very different response from other antidepressants, which must be taken for four to six weeks before any benefit is felt,” said Albott. The study also showed that the peak response occurs after the medication has already cleared the body. “We believe it sets off a cascade of nerve growth factors that lead to the improvement we see 24 hours after the infusion,” she noted. “That’s important because some people were concerned that when you are on ketamine, the resulting intoxication could be responsible for any improvement. The answer to that is no, the most improvement occurs when the drug is no longer in the system and there are no more intoxicating effects.”
Because the Yale research showed that participants returned to their depressed state a week to 10 days after the infusion, the U of M study is giving multiple infusions as a way to prolong the benefit, according to Albott. The median symptom improvement response was three weeks in the pilot study at the U.
That is the biggest downside of ketamine – it doesn’t last. “To maintain the benefit in the way we understand it today, you have to be on it for some time,” said Albott. “This is where some very interesting research questions come in…can we overlay psychotherapy with ketamine to perhaps get longer lasting benefit?”
Study protocol
The current study is titled, “Ketamine for Major Depressive Disorder and Post-traumatic Stress Disorder,” and plans to enroll 42 Veterans – half have already been recruited. There are risks associated with ketamine and everyone is informed about them, Albott noted. “We pre-screen for those risks, especially for comorbidities that would make using ketamine a problem,” she said. Comorbidities that would exclude Veterans from the study include epilepsy, heart disease, active suicidal thoughts, and recent history with substance use disorder.
Participants in the blinded, randomized study will undergo a series of baseline assessments, including the CAPS 5 (Clinician Administered PTSD Scale) and the Montgomery-Asberg Depression Rating Scale. They will also receive baseline functional magnetic resonance imaging (fMRI) and will then be randomized to receive either six ketamine or six normal saline infusions on a twice weekly schedule over three weeks.
Careful monitoring
On the day of infusion, participants will be required to stay at the clinical site for two hours after the infusion. “Due to the effects of ketamine, for safety people must have a driver after their treatment,” said Albott, who is present at all the infusions. The team will also call participants the day after the infusion to see how they’re doing.
An additional 21 participants will be enrolled in a healthy control group, and will undergo baseline assessments, including a single fMRI. All visits take place at the Minneapolis VA Medical Center, except for the MRI scans, which are done at the University of Minnesota Center for Magnetic Resonance Research (CMMR).
The research team created a safety plan that participants can follow if they have any worsening symptoms or feel like they’re de-compensating. “We haven’t had any issues because my study team is good about being in close regular contact with participants and keeping people well informed,” said Albott.
What’s really exciting
The fMRI data that indicates which brain networks improve as a result of the treatment is one of the most exciting — and time-consuming — aspects of the study, noted Albott. “There is some thought that when you’ve recovered, your brain will look like a normal brain,” she noted. “That may not be the case. We may be able to identify other compensatory mechanisms that are enabled by the treatment. This kind of finding would enable us to use less invasive treatments such as transcranial magnetic stimulation to upregulate the activity or to continue to change the network and keep people in recovery. That’s what is really exciting about this dataset.”