HOT History
"The measurement of progress against disorder is the control of disease in man. This requires research related to diagnosis, treatment, and prevention while at the same time emphasizing fundamental research."
- B.J. Kennedy
Through it all we remember the patients whose care is still imperfect, whose diseases are still misunderstood, and whose treatments could be improved. There are many model clinical investigators that have taught us many things, and they should not be forgotten. Welcome to the University of Minnesota Medical School, Department of Medicine, Division of Hematology, Oncology, and Transplantation (HOT). The HOT Division physicians, clinical, and research faculty are engaged in cutting-edge investigations aimed at understanding the causes of disease and translating that knowledge into better patient care, helping to save lives.
In 1998 Dr. Philip McGlave helped initiate a project to consolidate Hematology, Oncology, and Bone Marrow Transplant.
"To enhance the competitive relevance of programs that are geographically dispersed or in facilities that no longer support them by creating opportunities for physical consolidation and/or plans for renovation that will allow for more effective use of the space we have."
Prior to that time the HOT Division consisted of separate divisions within the Department of Medicine.
The Division of Medical Oncology, under BJ Kennedy, appointment as UMN faculty 1952. He is often referred to as the “Father” of Medical Oncology. BJ Kennedy was against using the word terminal in any reference to cancer patients.
The Division of Hematology, under Dr. Harry Jacob, 1968, was able to initiate a new hematology/oncology division at the University of Minnesota, which ultimately became a major center of productive research and a major teaching and fellowship training success.
Dr. Robert Alan Good, a founder of modern immunology and a pioneer in bone marrow transplantation. The first bone marrow transplant was conducted by Dr. Robert Good at the University of Minnesota in 1968. John Kersey, MD, was the founder of the UMN Blood and Marrow Transplantation (BMT) program, and performed the first successful bone marrow transplant to cure lymphoma.
“I think the most remarkable thing about the Hematology training program here at UofM has been it being an environment of faculty with remarkable creativity, that valued thinking outside of the box, that created an atmosphere such that not only was coming up with a crazy idea tolerated, rather it was encouraged and fostered. This is to be celebrated, as it is NOT a common occurrence in academic medicine settings. The faculty blend created an environment in which speculation was prized and dogmas questioned. I have always felt that unique environment (for that timeframe) created a special creativity-promoting milieu that contributed to so many fellows making so many important observations.”
– Dr. Robert P. Hebbel Regents Professor Emeritus
Milestones at Minnesota
1968: World’s first successful human BMT using an HLA matched sibling donor.
Robert Good, MD, led the team treating an infant with an immune deficiency syndrome.
1974: BMT program established at the University of Minnesota.
1975: First successful transplant in a patient with lymphoma.
1979: Adult BMT program established.
1980s: Development of autologous marrow transplantation—for chronic myelogenous leukemia.
1982: First transplant for an inherited metabolic disease.
1985: Unrelated donor transplant is initiated at University of Minnesota.
1991: First cord blood transplant using a related donor for a child with leukemia.
1992: Autologous BMT is used to treat breast cancer.
1994: First unrelated umbilical cord blood transplant.
1998: University of Minnesota Cancer Center, including the BMT program; NCI-designated Comprehensive Cancer Center.
1999: The 3,000th BMT is performed at University of Minnesota Medical Center.
1999: First sickle cell patient transplanted using a nonmyeloblative allogeneic sibling transplant.
2000: The first UCBT for Fanconi Anemia using pre-implantation genetic testing. This ensures a perfect tissue match.
2000: The first successful double-cord blood transplant.
2003: Successful engraftment of cord blood grafts for adults using two closely matched cord blood units.
2004: Reduced intensity UCB grafts for adults not suited for conventional allogeneic transplantation.
2004: Successful early experience of leukemia reinduction using haploidentical donor natural killer cells.
2007: 5,000th BMT is performed at University of Minnesota Medical Center.
2008: 40th anniversary of program.
2008: First-in-human trial of peripheral blood T-regulatory cells as a method to attempt to prevent GVHD.
2009: Clinical trial demonstrated that double UCBT (vs.single UCBT) reduces risk of relapse for patients with leukemia.
2009: Report of myeloablative double UCBT are equal to those of related or unrelated donor transplantation.
2010: Marrow stem cells and mesenchymal stem cells to repair the mucocutaneous disease, Epidermolysis Bullosa.
2015: Reports of successful Treg adoptive transfer to limit GVHD and maintain GVL
2016: Continuing study of NK cell infusions to limit risks of relapse
2017: Trial of IL-15 analogue (ALT-803) to prevent post HCT relapse
2017: 7500th BMT at the University of Minnesota
2018: 50th anniversary of program
2019: Broader donor options
2020: iPSC NK-CARs to limit relapse……..more to come
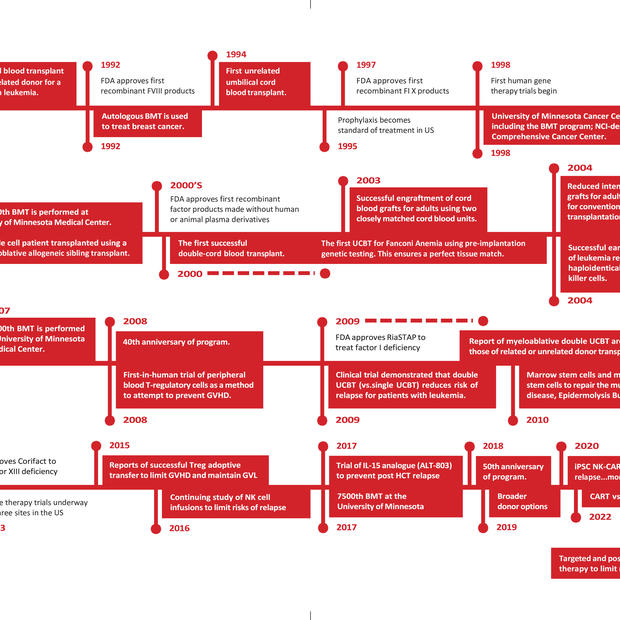
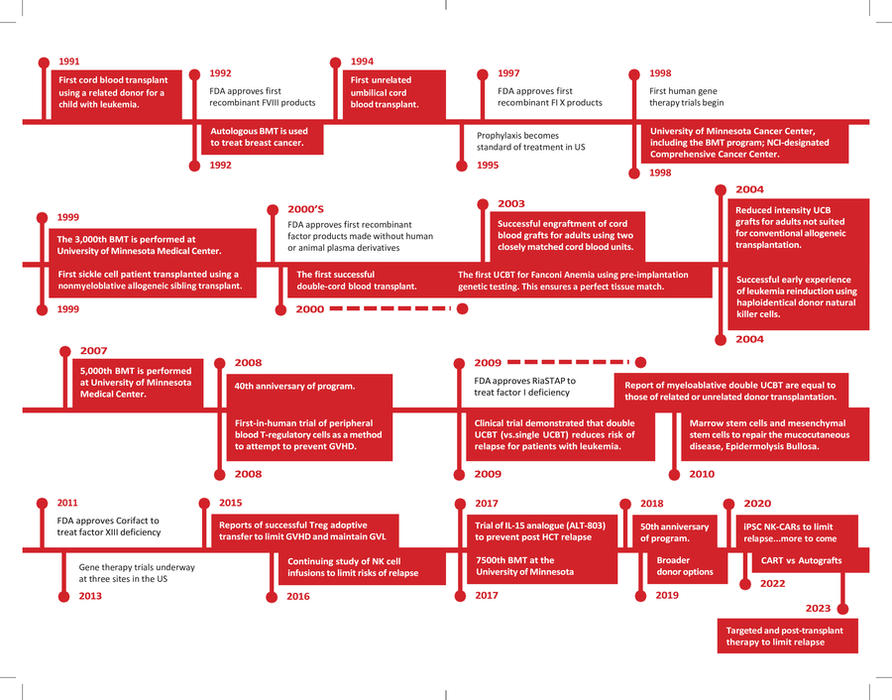
Timeline
Hematology, Oncology, Transplantation Timeline/Milestones
Year Discovery
1628 Discovery of the closed circulation of blood by William Harvey
1674 Description of RBCs by van Leeuwenhoek
1770-4 Discovery of WBCs, fibrinogen, the first anticoagulant (Glauber’s salt), and the fundamentals of blood coagulation and lymphatic circulation by Hewson
1818 First successful transfusion of human blood to a patient by Blundell
1828 Term “haemorrhaphilia” first used. Later shortened to “hemophilia.”
1832 First description of Hodgkin disease by Hodgkin
1840 First successful whole blood transfusion to treat hemophilia by Lane
1852-76 Development of RBC and WBC counting by hemocytometer by multiple investigators
1868 Discovery of the role of the bone marrow in hematopoiesis by Neumann and independently by Bizzozero
1868 Virchow describes leukemia, thrombosis, and embolism
1878 Blood cell staining developed by Ehrlich, followed by his identification of 3 types of granulocytes, mast cells, polychromatophilia, and megaloblasts
1882 First description of phagocytosis by Metchnikoff
1888 First description of the role of platelets in hemostasis and thrombosis by pathologist Giulio Bizzozero
1901 Discovery of blood groups, A, B, AB, and O (C) by Landsteiner
1903 First description of syndrome of polycythemia vera by Osler
1904 First description of paroxysmal cold hemoglobinuria by Donath and Landsteiner
1910 First description of bleeding time assay and effectiveness of platelet transfusion to treat thrombocytopenia by Duke
1910 First description of sickle cell disease by James Herrick
1915 Use of citrate to anticoagulant blood for transfusion optimized Richard Lewisohn
1918 First description of Glanzmann thrombasthenia by Glanzmann
1920 Classic description of infectious mononucleosis by Sprunt and Evans
1924 First description of Felty syndrome (association of chronic arthritis, splenomegaly, and leukopenia) by Felty
1925 First description of thalassemia by Cooley and Lee
1926 First description of von Willebrand disease by Erik von Willebrand
1926 Classic report of liver as first effective treatment of pernicious anemia by Minot and Murphy
1927 First description of Fanconi syndrome (pancytopenia, aplastic bone marrow, and physical anomalies) by Fanconi
1929 Hematocrit technique refined by Wintrobe, along with introduction of measure the size, shape, and quality of your red blood cells (RBC indices). Mean corpuscular volume (MCV) is a laboratory value that measures the average size and volume of a red blood cell. (MCH) stands for Mean Corpuscular Hemoglobin and is a calculation of the average amount of hemoglobin contained in each of a person's red blood cells. And (MCHC) is a measure of the concentration of hemoglobin in red blood cells.
1929 First description of sternal puncture to obtain bone marrow by Arinkin
1929 Identification of role of intrinsic factor in pernicious anemia by Castle
1934 Classification of anemias based on RBC indices by Wintrobe
1935 Development of the PT by Quick
1937 Identification of a globulin fraction of plasma as containing the atihemophiliac factor (later factor VIII) by Arthur Patek and FHL Taylor
1940’s Whole blood transfusions given at hospital
1941 First description of the effect of warfarin on the prothrombin time, sometimes referred to as PT or pro time, test is a test to evaluate blood clotting, in humans by Butt, Allen, and Bollman
1944 First description of macroglobulinemia by Waldenström
1945 The antihuman globulin test to identify “incomplete” antibodies developed by Coombs, Mourant, and Race
1946 Multiple reports of efficacy of nitrogen mustard compounds in lymphoma and leukemia by groups led by Goodman, Gilman, Jacobson, and Rhoads
1948 National Hemophilia Foundation (NHF) opens as The Hemophilia Foundation, Inc.
1950’s BJ Kennedy starting the Oncology Division UMN
1952 Researchers describe what is now called factor IX clotting protein
1954 NHF establishes a Medical Advisory Council, later called Medical and Scientific Advisory Council (MASAC)
1955 First infusions of factor VIII in plasma form
1957 Researchers in Sweden identify von Willebrand factor as the cause of VWD
1958 First use of prophylaxis for hemophilia A
1964 Dr. Judith Graham Pool discovers cryoprecipitate
1968 Hary Jacob, MD head of the Division of Hematology UMN
1968 First FVIII concentrate available
1968: World’s first successful human BMT using an HLA matched sibling donor. Robert Good, MD, led the team treating an infant with an immune deficiency syndrome UMN.
1970s Primary prophylaxis therapy experiments begin
1970s Freeze-dried plasma-derived factor concentrates available
1974 BMT program established at the University of Minnesota.
1975 First successful transplant in a patient with lymphoma.
1977 Desmopressin identified to treat mild hemophilia and von Willebrand disease
1979 Adult BMT program established.
1980s Factor VIII, FIX and von Willebrand factor genes cloned
1980s Development of autologous marrow transplantation—for chronic myelogenous leukemia.
1982 CDC reports first AIDS cases among people with hemophilia
1982 First transplant for an inherited metabolic disease.
1985 First inactivated factor concentrates available
1985 Unrelated BMT donor transplant is initiated at University of Minnesota.
1991 First cord blood transplant using a related donor for a child with leukemia.
1992 FDA approves first recombinant FVIII products
1992 Autologous BMT is used to treat breast cancer.
1994 First unrelated umbilical cord blood transplant.
1995 Prophylaxis becomes standard of treatment in US
1997 FDA approves first recombinant FIX products
1998 First human gene therapy trials begin
1998 University of Minnesota Cancer Center, including the BMT program; NCI-designated Comprehensive Cancer Center.
1999 The 3,000th BMT is performed at University of Minnesota Medical Center.
1999 First sickle cell patient transplanted using a nonmyeloblative allogeneic sibling transplant.
2000s FDA approves first recombinant factor products made without human or animal plasma derivatives
2000 The first UCBT for Fanconi Anemia using pre-implantation genetic testing. This ensures a perfect tissue match.
2000 The first successful double-cord blood transplant.
2003 Successful engraftment of cord blood grafts for adults using two closely matched cord blood units.
2004 Reduced intensity UCB grafts for adults not suited for conventional allogeneic transplantation.
2004 Successful early experience of leukemia reinduction using haploidentical donor natural killer cells.
2007 5,000th BMT is performed at University of Minnesota Medical Center.
2008 40th anniversary of program.
2008 First-in-human trial of peripheral blood T-regulatory cells as a method to attempt to prevent GVHD.
2009 FDA approves RiaSTAP to treat factor I deficiency
2009 Clinical trial demonstrated that double UCBT (vs.single UCBT) reduces risk of relapse for patients with leukemia.
2009 Report of myeloablative double UCBT are equal to those of related or unrelated donor transplantation.
2010 Marrow stem cells and mesenchymal stem cells to repair the mucocutaneous disease, Epidermolysis Bullosa.
2011 FDA approves Corifact to treat factor XIII deficiency
2013 Gene therapy trials underway at three sites in the US
2015 Reports of successful Treg adoptive transfer to limit GVHD and maintain GVL
2016 Continuing study of NK cell infusions to limit risks of relapse
2017 Trial of IL-15 analogue (ALT-803) to prevent post HCT relapse
2017 7500th BMT at the University of Minnesota
2018 50th anniversary of program
2019 Broader donor options
2020 iPSC NK-CARs to limit relapse...more to come
2022 CART vs Autografts
2023 Targeted and post-transplant therapy to limit relapse