Curriculum
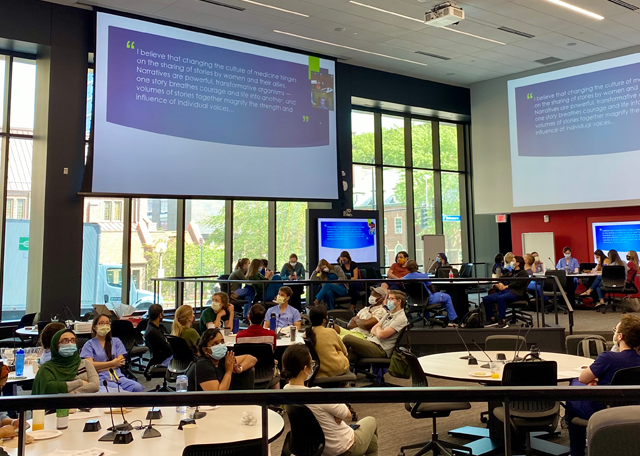
Resident conferences are a true strength of our program - they are high quality and very well attended. Some of the highlights include:
Example Schedule By Year
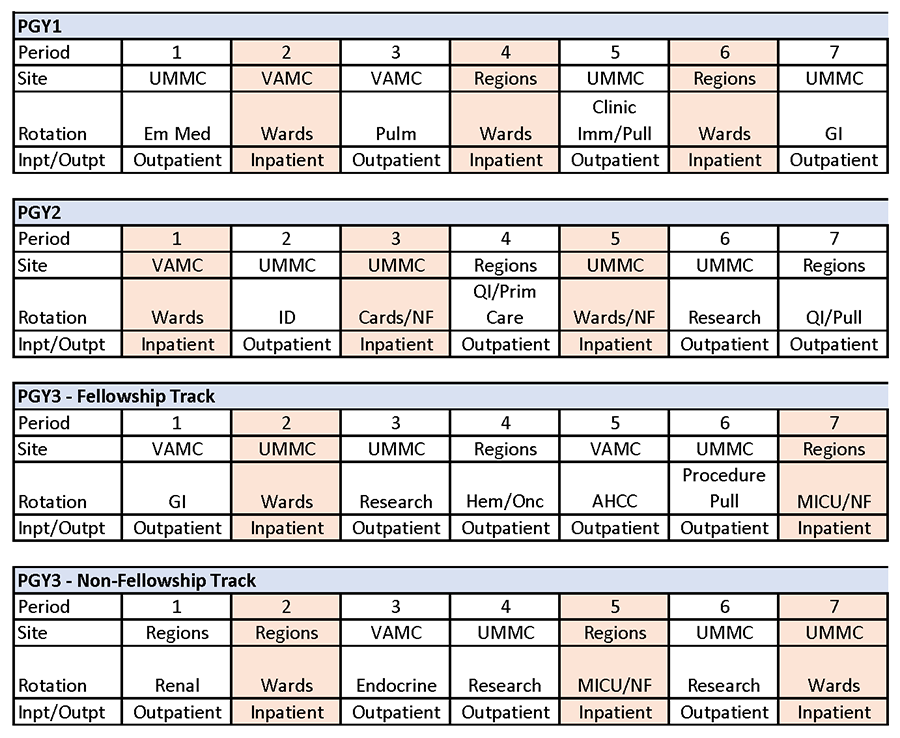
ROTATION STRUCTURE
We follow a 50/50 structure, which is a modified version of the 4+4 schedule. All of our rotations have night float; our residents do not have 24 hour shifts.
|
Rotation requirements by Year of Training (1 period=4 weeks) |
| PGY-1 |
|
| PGY-2 |
|
| PGY-3 |
|
ELECTIVES
UMMC: Addiction Medicine, Cardiology Elective, Consult and Procedure Service, Dermatology, Endocrinology, Emergency Medicine, Global Medicine, Heme Onc and BMT, Hospitalist, Infectious Disease, International Rotations, GI Consults and Outpatient Clinic, Nephrology Consults and Outpatient Clinic, Palliative Care, Pulmonology Consults and Outpatient Clinic, QI Didactics/Experiential, Research Rotations, Rheumatology, Ultrasound, Women’s Health
Regions: Cardiology Consults and Outpatient Clinic, Critical Care Elective, Emergency Medicine, Gastroenterology, Geriatrics, Global Health, Heme Onc Consults and Outpatient Clinic, Hospitalist, Infectious Disease, Multispecialty Outpatient Clinic, Nephrology, Palliative Care, Pulmonology, QI Didactics/Experimental, Rheumatology, Sports Medicine, Toxicology, Travel Medicine
VAMC: Cardiology Elective, Dermatology, Emergency Medicine, Endocrinology Consults and Outpatient Clinic, GI Consults and Outpatient Clinic, Geriatrics, Heme Onc, Infectious Disease, Multispecialty Outpatient Clinic, Palliative Care, Pulmonology Consults and Outpatient Clinic, Nephrology, Rheumatology, Sleep Medicine, QI Didactics/Experiential, Women’s Health
Morning report: Chief residents lead case-based discussion on a variety of core medical topics and interesting cases to enhance learning. This conference is attended by medical students, residents, and faculty to create an optimal learning environment for developing clinical management skills and medical knowledge. Cases are archived online for residents to review at their convenience.
Morbidity and Mortality: Chief residents direct a process-oriented approach to a clinical case with emphasis on pitfalls in diagnostic reasoning and important topics in quality improvement or systems-based issues. Expertise is provided by teaching faculty, including an array of sub-specialists. Each site conducts its own M&M series so residents are able to attend this conference regularly, regardless of the current site they are rotating at.
Grand Rounds: Specialty experts discuss cutting-edge research topics and clinical advancements in didactic sessions. Each clinical site has its own Grand Rounds series which residents are able to attend.
Continuity Clinic Conference: Preceptors and residents lead interactive, case-based teaching sessions on ambulatory topics during each continuity clinic. Cases are shared electronically with residents for future reference.
Other miscellaneous conferences: Residents have the ability to participate in a variety of other conferences including Schwartz rounds, combined EM/IM case conference and research conferences.
Communication Assessment and Skills Exercise (CASE)
This OSCE-format workshop was developed for new interns to practice delivering bad news, discussing code status, and dealing with angry patients in a safe, supportive environment.
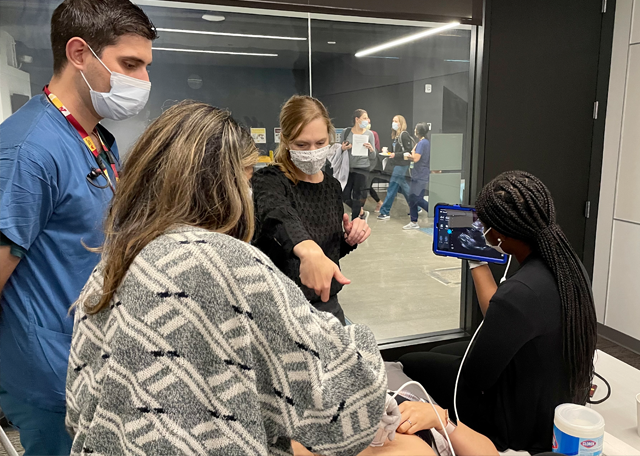
Introduction to Ultrasound
This introductory course includes directly-observed simulation in central line placement, radial artery line placement, thoracentesis/ chest tube placement, and paracentesis. It also includes hands-on instruction in the FAST exam, pulmonary and pleural evaluation (including lung sliding, pleural effusions, A-lines, and B-lines), and basic ultrasound assessment of the heart and great vessels (including contractility, pericardial effusion, and inferior vena cava size and variability) among other clinically useful assessments.
BLS/ACLS
Interns spend two days receiving training and certification in both basic and advanced life support.
IMED is a monthly academic half-day designed to cover essential topics and skills paramount to a career as an internist. IMED sessions utilize a variety of didactic techniques including small group discussions, procedural practice, and problem based learning. Intern and senior residents have separate sessions to help tailor learning across training levels. The curriculum is designed to be a longitudinal series without repeated content, and time is fully protected to ensure residents can fully immerse themselves in learning without the distraction of clinical responsibilities. Completion of the IMED curriculum will arm residents with a solid knowledge base for a variety of internal medicine conditions and provide explicit training in areas such as professionalism, implicit bias, high value care, and more to ensure residents emerge from training well-rounded providers.
Intern Curriculum
Intern sessions focus on improving the basic fund of knowledge and management of critical and common inpatient and outpatient conditions.
Sessions Include:
-
Intern 101: Efficiency, cross cover and other high yield topics
-
Common Critical Care
-
Primary Care 101
-
Benign Hematology
-
Common Infectious Disease
-
Dyspnea Part 1
-
Research
-
Abdomen, part 1 (part 2 as a senior resident)
-
Palliative Care, part 1 (part 2 as a senior resident)
-
Emergencies as a Resident
-
Social and Health Disparities
-
Professionalism Workshop
Residents and faculty discuss uncomfortable experiences encountered as physicians -- touching on racism, sexism, and health equity -- and discuss strategies to raise our profession to a higher standard. -
Essentials of Ambulatory Care Workshop
This is a multidisciplinary workshop with members from various other specialties (Family Medicine, Pediatrics, Pharmacy, NP, nursing) during which we discuss the medical and administrative skills needed to provide exemplary ambulatory care. -
Transition Workshop
This a year-end workshop for interns who are about to take on the role of senior resident, focusing on developing leadership skills and effective teaching techniques.
Senior Curriculum
Senior sessions work to expand knowledge of less common pathology, build on and refine management of complex patients, and develop skills related to leadership and interprofessional team building. The senior curriculum is a two year curriculum so every senior resident will see each session once during their second and third years.
Sessions Include:
-
Women’s Health, parts 1 and 2
-
Pain Assessment and Chronic Pain Management
-
Dyspnea, parts 1 and 2
-
General Cardiology, parts 1 and 2
-
Abdomen, part 2 (part 1 as an intern)
-
Palliative Care, part 2 (part 1 as an intern)
-
Common Dermatology
-
Neurology
-
Mental Health
-
Malignant Hematology
-
Renal
-
Endocrinology
-
Board Study
-
Infectious Disease in Transplant and Immunocompromised Patients
-
Wellness and High Value Care
-
Pediatrics to Adult Transitions (Med-Peds Focus)
-
Leadership and Communication Workshop
The first half of this workshop is focused on understanding how personality and temperament influences different leadership styles and how that plays into creating an effective team. It also involves residents setting their own personal goals around leadership development. The second half of the workshop is focused on communication. This involves learning how our own biases can impact the learner experience, performance and evaluation and learning tools to mitigate bias in feedback and evaluations. -
Job Negotiation Workshop
This workshop is focused on helping residents develop an understanding of negotiation as part of the job search process and well as in periodic career opportunities. It also includes a panel conversation on finances, loan repayment and retirement planning. -
ACLS/BLS Renewal
The University of Minnesota offers a curriculum in medical procedures and in diagnostic point-of-care ultrasonography in which all Internal Medicine, Medicine-Pediatrics, and Medicine-Dermatology residents participate beginning their intern year.
Our introductory course includes directly-observed simulation in central line placement, radial artery line placement, thoracentesis/ chest tube placement, and paracentesis. It also includes hands-on instruction in the FAST exam, pulmonary and pleural evaluation (including lung sliding, pleural effusions, A-lines, and B-lines), and basic ultrasound assessment of the heart and great vessels (including contractility, pericardial effusion, and inferior vena cava size and variability) among other clinically useful assessments. All incoming interns take this course as part of intern orientation
An Advanced Ultrasound Course is offered as an elective to senior residents two times per year. The course focuses on diagnostic point-of-care ultrasound, and reinforces many of the concepts from the introductory course; as well as integrating these ideas into the workup of hypotension, dyspnea, and assessment of intravascular volume. Interested resident can also learn evaluation for lower extremity deep venous thrombosis and abdominal aortic aneurysms. A significant portion of the course is spent scanning a large number of patients admitted to UMMC and building portfolios demonstrating ability to acquire and interpret images
An inpatient medicine Consult and Procedure Service (CAPS) offers paracentesis, thoracentesis, and lumbar punctures. This is a two week rotation available to senior residents as an elective. Resident continue to learn procedures on other rotations as well, and perform procedures and Regions Hospital and the VAMC. If a resident wishes to take both the Advanced Ultrasound Course and CAPS rotation, the resident would ideally take the advanced course first, as extra time on the CAPS service may then be used for additional portfolio building
Internal Medicine Residency Program Scholarly Activity
An important part of residency training is scholarly activity. Our program supports this by providing all interns with 5 days a year for professional development, $200 for academic expenses, and a subscription for MKSAP and ACP membership. As senior residents, all residents have $600 each year for academic expenses. PGY2 residents also have 5 days a year for professional development, and PGY3 residents have 10 days a year for professional development. All of our residents can also take an additional day each year for advocacy or volunteer work.
Possible Experiences as a Resident
- Participating in clinical, educational, or basic science research
- Presenting an interesting clinical case at fall Minnesota ACP (usually held in downtown Minneapolis)
- Presenting a poster at Department of Medicine Research Day in the spring
- Presenting an abstract at a national or international subspecialty conference, such as CHEST, DDW, ASCO, or ACC meeting.
- Attending workshops or presenting at Midwest SGIM (Society for General Internal Medicine) or CGEA (Central Group on Educational Affairs), held every spring at a Midwest location
- Publishing a case report, abstract, or original research