
Center for Red Cell Disorders
Mission
As part of the University of Minnesota’s Red Cell Disorder Program, the Sickle Cell Disease (SCD) Program strives to provide exceptional evidence-based and anti-racist care for individuals with SCD and related blood disorders. As the only institution in the Twin Cities dedicated to providing lifespan SCD care, we prioritize patient values and inclusivity in decision making while advancing sickle cell care, especially in the transition to adulthood. This includes conducting bench, translational, and clinical research and offering cutting-edge curative therapies in our continued vision for growth and excellence for our patients and their families.
Services
As statewide leaders in advancing SCD clinical care and research and a recognized pediatric and adult SCD center by the National Association of Sickle Cell Centers (NASCC) with over 200 patients, we strive to provide holistic and comprehensive care for patients of all ages. Our providers also work regularly with national leaders and participate in various committees within the American Society of Hematology to advance SCD care nationally and globally.
We have two pediatric physicians, two pediatric nurse practitioners, a nurse care coordinator, and a social worker providing pediatric SCD care. In our adult program, we have eight physicians providing both inpatient and outpatient SCD care along with three physician assistants, five nurse care coordinators, a patient intake coordinator, and social workers. We have strong collaborations with pain management specialists, maternal-fetal medicine/obstetrics and gynecology, primary care providers, pulmonology, cardiology, orthopedics, ophthalmology, and other specialists. We also collaborate with Dr. Ashish Gupta, MBBS, MDH, in addition to adult hematologist Roy Kao, MD, to provide access to curative therapies, including hematopoietic stem cell transplantation and active trials in gene therapy. Because of our cutting-edge program, we are the primary referral center for Minnesota, Iowa, North Dakota, South Dakota, and western Wisconsin.
We provide infusion clinic access five days a week for pain medications, crizanlizumab, and blood products as needed. We also have regular coordination with the emergency department, primary care, and various specialty providers for all ages.
A prioritized area of expertise for our program is in the adolescent and young adult (AYA) transition period of SCD care under the lead of Dr. Boucher, who is nationally recognized for his work in this area. We have multiple physicians and nurse practitioners who have developed experience in the unique aspects of helping patients and families gain comfort and familiarity with the differences in adult care as compared to their previous pediatric programs. Our most rapid growth has been with individuals 30 years and younger who have sought out the continuity of care we provide within our program. We not only try to optimize patient care for AYA individuals with SCD but we are also conducting patient-centered clinical research on improving transitions to be an example nationally of how successful transitions can be done.
Education
The University of Minnesota medical center has long prioritized education for medical trainees, colleagues, patients, and their families. We have a Hematology-Focused Fellowship Training Program; one of only 9 academic centers funded by the American Society of Hematology (ASH) to train the next generation of hematologists. For SCD specifically, we provide regular education for medical students, residents, clinical fellows, pharmacists, advanced practice providers (APPs), and nurses through medical school programming, mixed methods of adult learning strategies, and a nationally funded grant for a Patient-Centered Outcomes Research Institute (PCORI) to enhance nursing and APP education within our infusion clinic. Drs. Datta, Vercellotti, Boucher, and Mazepa lead local curricula and fellowship programs and Dr. Boucher works closely with ASH on medical education for trainees with a particular focus on health equity and advancing SCD knowledge and care to primary care clinics and hospital providers.
Center for Red Cell Disorders Faculty
|
Pediatrics Alex Boucher, MD Karim Sadak, MD Kelsey Olsen, PNP Erin Fritz, PNP Anna Tan, RN Emily Villanueva, MSW, LGSW Ashish Gupta, MBBS, MPH (Bone Marrow Transplant/Cellular Therapy) |
Adult Alex Boucher, MD Greg Vercellotti, MD Roy Kao, MD (Including Bone Marrow Transplant/Cellular Therapy) Jacob Cogan, MD Yvonne Datta, MD Mark Reding, MD Joan Beckman, MD Marshall Mazepa, MD Emily Peeler, RN Cindy Heitland, RN Maureen Collins-Fuchs, RN Makayla Brummer, RN Sara Wojciechowski, RN Pam Peterson, RN (New Patient Intake) Tenzin Lhadon, LICSW |
Basic and Clinical Research group Greg Vercellotti, MD John Belcher, PhD Joan Beckman MD, PhD David Wood, PhD Alex Boucher, MD, Roy Kao, MD Ashish Gupta, MBBS, MPH |
Center for Red Cell Disorders Clinical Trials
UMN-initiated Studies
-Young Adult New Patient Integration Trial
National and Regional Studies/Databases
https://med.umn.edu/dom/divisions/hematology-oncology-and-transplantation/clinical-trials
-Patient-Centered Outcomes Research Institute (PCORI) study to improve infusion clinic experience for patients
-Recently completed Phase 1 Trial of CSL889 for new SCD drug therapy
-Multiple gene therapy trials for curing SCD.
-Involvement in national SCD data registry as part of NASCC
-Consultant for the Minnesota Department of Health’s CDC Grant to understand statewide patterns in SCD care
Basic Science and Clinical Research
For over 45 years, University of Minnesota researchers have been dedicated to understanding the pathophysiology of SCD. Dr Robert Hebbel's paradigm-shifting studies of sickle red blood adhesion to the vessel wall and inflammation leading to ischemia-reperfusion physiology led to modern therapies for SCD. Dr. Kalpna Gupta pioneered studies on pain in SCD leading to new pain therapies. Presently, Dr. Greg Vercellotti and Dr. John Belcher have focused on mechanisms of vaso-occlusive pain crises and the role of hemolysis, inflammation, oxidative stress and complement. Their pre-clinical studies have led to the approval of 4 new drugs in Phase 1-2 clinical trials to modify vaso-occlusion. Their present work on complement activation in pain in SCD continues along with basic research on gene therapy in SCD.
Dr. Alex Boucher has been site primary investigator of an international Phase 1 trial on hemopexin in SCD. Dr. Joan Beckman has examined how carbon monoxide and heme oxygenase can modulate vaso-occlusion. Her present studies on TLR4 and HDAC-6 inhibitors will provide new avenues for treatment of SCD. Dr. David Wood in Biomedical Engineering collaborates with Drs. Vercellotti, Beckman, and Datta to better understand how treatments and therapies can improve the lives of individuals with SCD. He devised a microfluidic device that can mimic vaso-occlusive events. This has been utilized to monitor the effect and success of gene therapies in SCD patients.
Selected Publications
University of Minnesota Sickle Cell Disease Publications
- Ivy ZK, Belcher JD, Khasabova IA, Chen C, Juliette JP, Abdulla FR, Ruan C, Allen K, Nguyen J, Rogness VM, Beckman JD, Khasabov SG, Gupta K, Taylor RP, Simone DA, Vercellotti GM. Cold exposure induces vaso-occlusion and pain in sickle mice that depend on complement activation. Blood. 2023 Sep 29:blood.2022019282. doi: 10.1182/blood.2022019282. Online ahead of print. PMID: 37774369
- Beckman JD, Sparkenbaugh EM. The invisible string of coagulation, complement, iron, and inflammation in sickle cell disease. Curr Opin Hematol. 2023 Sep 1;30(5):153-158. doi: 10.1097/MOH.0000000000000773. Epub 2023 Jul 14. PMID: 37462409
- Boucher AA, Lyons M, McGann PT. Rethinking Care Models for Young Adults With Sickle Cell Disease. JAMA Health Forum. 2023 May 5;4(5):e230877. doi: 10.1001/jamahealthforum.2023.0877. PMID: 37171796
- Belcher JD, Nataraja S, Abdulla F, Zhang P, Chen C, Nguyen J, Ruan C, Singh M, Demes S, Olson L, Stickens D, Stanwix J, Clarke E, Huang Y, Biddle M, Vercellotti GM. The BACH1 inhibitor ASP8731 inhibits inflammation and vaso-occlusion and induces fetal hemoglobin in sickle cell disease. Front Med (Lausanne). 2023 Apr 18;10:1101501. doi: 10.3389/fmed.2023.1101501. eCollection 2023. PMID: 37144034
- Khasabova II, Juliette J, Rogness VM, Khasabov SG, Golovko MY, Golovko SA, Kiven S, Gupta K, Belcher JD, Vercellotti GM, Seybold VS, Simone DA. A model of painful vaso-occlusive crisis in mice with sickle cell disease. Blood. 2022 Oct 20;140(16):1826-1830. doi: 10.1182/blood.2022017309. PMID: 35960856
- Azul M, Vital EF, Lam WA, Wood DK, Beckman JD. Microfluidic methods to advance mechanistic understanding and translational research in sickle cell disease. Transl Res. 2022 Aug;246:1-14. doi: 10.1016/j.trsl.2022.03.010. Epub 2022 Mar 27. PMID: 35354090
- Gentinetta T, Belcher JD, Brügger-Verdon V, Adam J, Ruthsatz T, Bain J, Schu D, Ventrici L, Edler M, Lioe H, Patel K, Chen C, Nguyen J, Abdulla F, Zhang P, Wassmer A, Jain M, Mischnik M, Pelzing M, Martin K, Davis R, Didichenko S, Schaub A, Brinkman N, Herzog E, Zürcher A, Vercellotti GM, Kato GJ, Höbarth G. Plasma-Derived Hemopexin as a Candidate Therapeutic Agent for Acute Vaso-Occlusion in Sickle Cell Disease: Preclinical Evidence. J Clin Med. 2022 Jan 26;11(3):630. doi: 10.3390/jcm11030630.
- Hebbel RP, Vercellotti GM. Multiple inducers of endothelial NOS (eNOS) dysfunction in sickle cell disease. Am J Hematol. 2021 Nov 1;96(11):1505-1517. doi: 10.1002/ajh.26308. Epub 2021 Aug 23. PMID: 34331722
- Zhang P, Nguyen J, Abdulla F, Nelson AT, Beckman JD, Vercellotti GM, Belcher JD. Soluble MD-2 and Heme in Sickle Cell Disease Plasma Promote Pro-Inflammatory Signaling in Endothelial Cells. Front Immunol. 2021 Mar 26;12:632709. doi: 10.3389/fimmu.2021.632709. eCollection 2021. PMID: 33841413
- Azul M, Shah S, Williams S, Vercellotti GM, Boucher AA. Evidence for complement-mediated bone marrow necrosis in a young adult with sickle cell disease. Blood Cells Mol Dis. 2021 Feb;86:102508. doi: 10.1016/j.bcmd.2020.102508. PMID 33096468
- Beckman JD, Abdullah F, Chen C, Kirchner R, Rivera-Rodriguez D, Kiser ZM, Nguyen A, Zhang P, Nguyen J, Hebbel RP, Belcher JD, Vercellotti GM. Endothelial TLR4 expression mediates vaso-occlusive crises in sickle cell disease. Front Immunol. 2021 Jan 19;11:613278. doi: 10.3389/fimmu.2020.613278. eCollection 2020. PMID: 33542720
- Hebbel RP, Belcher JD, Vercellotti GM. The multifaceted role of ischemia/reperfusion in sickle cell anemia. J Clin Invest. 2020 Mar 2;130(3):1062-1072. doi: 10.1172/JCI133639. PMID: 32118586
- Gupta K, Chen C, Lutty GA, Hebbel RP. Morphine promotes neovascularizing retinopathy in sickle transgeneic mice. Blood Adv. 2019 Apr 9;3(7):1073-1083. doi: 10.1182/bloodadvances.2018026898. PMID: 30944099
- Vercellotti GM, Khan FB, Nguyen J, Chen C, Bruzzone CM, Bechtel H, Brown G, Nath KA, Steer CJ, Hebbel RP, Belcher JD. H-ferritin ferroxidase induces cytoprotective pathways and inhibits microvascular stasis in transgenic sickle mice. Front Pharmacol. 2014 Apr 17;5:79. doi: 10.3389/fphar.2014.00079. eCollection 2014. PMID: 24860503
- Belcher JD, Chen C, Nguyen J, Milbauer L, Abdulla F, Alayash AI, Smith A, Nath KA, Hebbel RP, Vercellotti GM. Heme triggers TLR4 signaling leading to endothelial cell activation and vaso-occlusion in murine sickle cell disease. Blood. 2014 Jan 16;123(3):377-90. doi: 10.1182/blood-2013-04-495887. Epub 2013 Nov 25. PMID: 24277079
Media
“Consider Mental Health and Social Factors in Management of Sickle Cell Disease”, with Heidi Splete, MDEdge (Medscape) internet article interview (6/22/23)
“Living SickleSMART: Curative Therapies in Sickle Cell Disease.” Sickle Cell Foundation of Minnesota video interview (Kao, Gupta) (4/26/23)
“Getting people to care about sickle cell when it’s considered ‘only a Black disease’", MinnPost, magazine interview (2/10/23)
“Minnesotans raise awareness of sickle cell anemia.” CBS News Minnesota (WCCO) television interview (9/28/22)
“Living SickleSMART: Let’s Talk Transition.” Sickle Cell Foundation of Minnesota video interview (Boucher) (12/3/21)
Organizational Chart
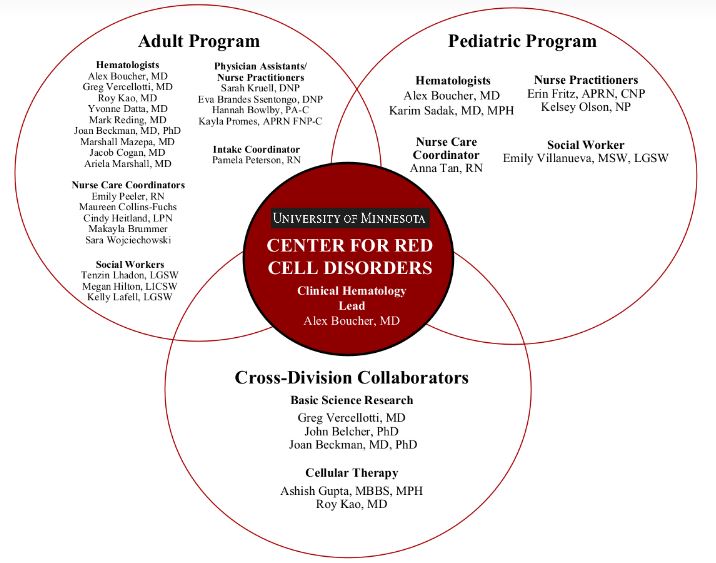
Sickle Cell Disease Program Director
Pediatric and Adult care
Community Involvement
Our providers work closely with
the Sickle Cell Foundation of
Minnesota and the Minnesota
Department of Health
Program) to improve patient
and family experiences and
outcomes, understand the
current use of medical care
for those affected by SCD,
and ensure community
involvement to advance our
education, research, and
patient-centered outcomes.