Sickle Cell Comprehensive Care Program
Sickle cell disease (SCD) is a disorder characterized by abnormal protein in your red blood cells that carries oxygen to your body's organs and tissues and transports carbon dioxide from your organs and tissues back to your lungs. An estimated 100,000 people in the United States live with this chronic multi-systemic disease. The underlying science and predictable inheritance patterns of a single gene disease like SCD has long been known. The first discovery of SCD made in western medicine happened in 1910 by a Chicago physician Dr. James Herrick. He published about a blood sample that showed “sickle-shaped and crescent-shaped” red blood cells about an individual, who was severely anemic and experiencing pain episodes. Years later Linus Pauling named SCD as the first molecular disease in 1949.
Despite the improved scientific understanding surrounding the pathophysiology of SCD, the advancement in therapies and commitment to care for those affected by this serious and often debilitating disease has been sluggish. This can in part be explained by the varied observable characteristics in individual expressions within the same genetic makeup. However, understanding the mechanisms of SCD does not explain the health care response that has existed for SCD. Compared to other chronic inherited diseases that are not as common, patients and families affected by SCD have experienced far less access to care and limited access to research initiatives that would advance this care. This is a concern as survival of adults with SCD even in developed countries is significantly decreased, by 20 to 30 years, compared with unaffected similar persons.
Despite these barriers and disparities, there is reason to believe that change is coming. There have been recent drug approvals with additional treatments being studied. Also, clinical trials investigating curative therapies are ongoing. Prominent agencies and organizations are taking special interest in SCD and mounting initiatives to advance care and research. Though these recent changes are encouraging, one should not become complacent. Patients affected by SCD remain threatened by the risk of poor outcomes and early mortality due to lack of therapeutic options and limited access to experienced, patient-centered care.
Improving Quality of Life for People with SCD

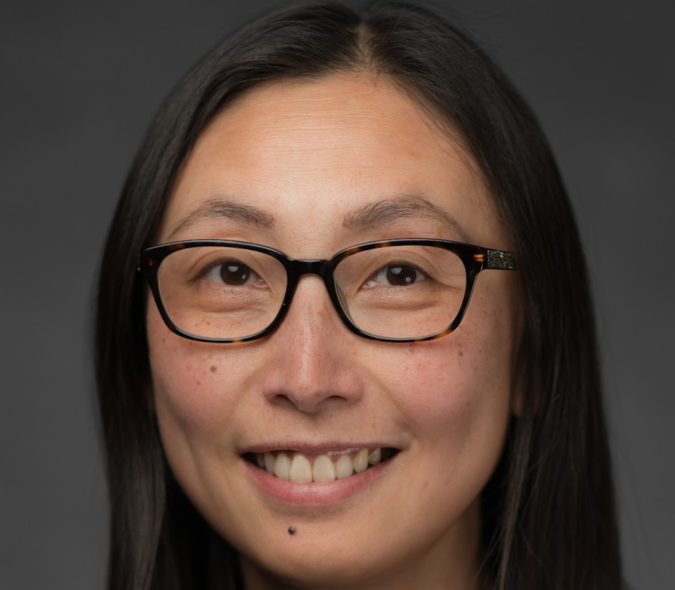
“At the University of Minnesota, we are engaged in cutting-edge bench-to-bedside research, including working to cure SCD,” said Dr. Alex Boucher, an assistant professor at the University of Minnesota Medical School, Division of Hematology, Oncology, and Transplantation. “We are simultaneously working with multidisciplinary medical teams to provide a more equitable, transparent and holistic approach to care across our system.” Dr. Boucher is nationally recognized for his work in this area serving as the Sickle Cell Disease Program Director Pediatric and Adult care, Center for Red Cell Disorders, as the primary referral center for Minnesota, Iowa, North Dakota, South Dakota, and western Wisconsin.
Dr. Boucher has been fully engaged with clinical, research and teaching interests revolving around rare inherited blood disorders, especially SCD and similar blood disorders passed down through families, in which the body makes an abnormal form or inadequate amount of hemoglobin. His passion is to care for SCD and similar disorders in a way that embraces quality medical care while expanding clinical research opportunities for patients and families, with an emphasis in patient-centered outcomes, transparency in care, and health equity. Dr. Boucher highlights trust and good rapport with each patient and family throughout their lifetime as foundational to growing a sustainable program.
“While there is excitement around curative therapies for sickle cell disease, and appropriately so, this is only an option for a small subset of patients right now,” said Boucher. “But a large majority of individuals with sickle cell disease will need emergency care for disease complications, and they want and deserve to be trusted by the medical system. Building that trust and building those individual connections with each patient, that’s what we aim to do before anything else.”
A Comprehensive View for Wide Ranging Care

The University of Minnesota is the largest system to provide lifespan sickle cell care in the state and the only one in the Metro area. We are also the only site in the region to offer curative therapy for sickle cell disease and thalassemia, including bone marrow transplant and gene therapy.
Dr. Boucher is working with colleagues to continue integrating other specialties including primary care, reproductive care, and mental health, so that patients can conveniently access all their care needs in one place and with providers who are experts in working with sickle cell disease. Dr. Boucher has been contributing to an ongoing Phase 1 multinational trial for a first-in-human drug trial, Safety of Single Doses of CSL889 in Adult Patients with Sickle Cell Disease. The foundational basic science work for this trial is done at the University of Minnesota and the trial has an active patient population that has nearly doubled in four years.
Minnesota is one of twelve states that are working to improve the quality of life for individuals and communities affected by SCD as part of the national CDC Sickle Cell Data Collection (SCDC) a program that gathers health information about people with SCD to study continuing trends in diagnosis, treatment, and healthcare access for people with SCD in the United States. To effectively service SCD patients, the program helps to inform policy and healthcare standards that advance and prolong the lives of people with SCD. The road to changing the sickle cell narrative is through developing key partnerships with the SCD and medical communities and working together to learn more about the experiences of living with SCD in Minnesota.
Dr. Boucher serves as a consultant for the Minnesota Department of Health's grant from the CDC to gather statewide data on sickle cell care utilization. “Despite this growth in the active SCD patient population,” said Dr. Boucher, “we have seen major reductions in the number of times our patients have to seek emergency care or be admitted to the hospital and reduced length of stay in the past four years. We have done this by working to expand access to our infusion clinic and by enhancing the approach to all-around preventive healthcare for our patients.” Dr. Boucher is working with colleagues on patient-centered outcomes research which is ongoing in a national multi-site study (optimizing infusion clinic care) and an investigator-led institutional trial on improving transitions to adult care.
Dr. Boucher’s work continues to bring perspective to the SCD community, both as a leader who has navigated the sickle cell space of the healthcare system and from his unique experience inside the system as part of the clinical care team for both children and adults. It is through this dual lens that Dr. Boucher continues to help and influence the path of many individuals, families, and professionals, all of whom command a critical role in improving the outcomes of the SCD population. “We can always do better,” said Dr. Boucher. “That’s certainly the case for chronic diseases of childhood, like sickle cell disease, as with most patients, they’re living with this for life and we need to provide patients with a sense of trust that we are listening to them.”
Dean Patterson, Editor
Division of Hematology, Oncology, and Transplantation
References
CDC Sickle Cell Data Collection https://www.cdc.gov/ncbddd/sicklecell/
Azul M, Shah S, Williams S, Vercellotti GM, Boucher AA. Evidence for complement-mediated bone marrow necrosis in a young adult with sickle cell disease. Blood Cells Mol Dis. 2021 Feb;86:102508. doi: 10.1016/j.bcmd.2020.102508. Epub 2020 Oct 9. PMID: 33096468; PMCID: PMC7546691.