Methodist Curriculum and Call
Methodist residents provide comprehensive and continuous care for their own panel of patients.
First-year residents spend one day in clinic per week. Second- and third-year residents spend four or five half-days in clinic per week.
Below you will find more information about our curriculum and call.
Rotations
Tailored to resident interests, and electives are chosen from standing rotations or developed to meet specific needs.
Longitudinal experiences
Includes noon conferences and curriculum in behavioral medicine, community health, geriatrics, and more.
Global Health
Opportunities include international and global-local electives, courses, seminars, conferences, and fellowship.
Lead resident and assistant lead residents
The lead resident is a one-year elected, salaried position, occupied by a third-year resident. Each third-year resident rotates as assistant lead for a two- or three-month period.
Programmatic courses
The department sponsors several required and optional one- to two-day programmatic courses. Topics include women's health, sports and musculoskeletal medicine, community health, and more.
Evaluation
Information regarding evaluation of residents
Call
View call information for each year of residency.
Residents As Teachers
Family medicine residents are directly responsible for a portion of medical student clinical education during clinical experiences and clerkships.
Medical education features a closely connected cycle of teaching, learning, and progressive responsibilities; senior learners teach junior learners, and all learners are involved in ongoing professional and personal development.
Residents of the eight University of Minnesota family medicine residency programs have many responsibilities, including that of supervisors and educators. Most medical students encounter family medicine residents as teachers during the Family Medicine Clerkship. Therefore, residents receive instruction about clerkship/rotation goals and objectives as well as training in teaching methods.
Resources
Resources are available to aid residents in development as teachers.
- Residents Teaching Students: Developed by family medicine medical student education director David Power, MBBS, MPH, and colleagues, it provides an overview of several teaching strategies. One of these is a common teaching method used by both residents and faculty, known as the One Minute Preceptor.
- Resident Educator Development and corresponding Moodle site: Assembled by the University’s Internal Medicine Residency Program and Office of Graduate Medical Education.
- Faculty advisors and residency directors also can connect residents with resources to enhance teaching abilities.
First Year
CARDIOLOGY 1
Setting: One month inpatient rotation at Methodist Hospital with cardiology staff
Learning: Inpatient cardiology consults, EKG reading, echocardiography, stress tests, cardiac MRI, angiography
CRITICAL CARE
Setting: One month rotation at Methodist Hospital with critical care staff
Learning: Management of common critical care conditions such as acute respiratory failure and fundamentals of ventilator management, acute renal failure and determining the need for dialysis, sepsis and shock, acute GI hemorrhage, diabetic ketoacidosis, and others
EMERGENCY MEDICINE
Setting: One month inpatient rotation in the Methodist Hospital emergency department with emergency physicians
Learning: Triage of acutely ill patients, evaluation and management of typical emergency room visits, suturing
FAMILY MEDICINE INPATIENT
Setting: A total of three months of inpatient family medicine at Methodist Hospital
Learning: Admission, management, and discharge of typical hospital patients, daily sit-down rounds, and presentation required by the team at a noon conference based on a case seen during the month
NEUROLOGY
Setting: One month mixed inpatient/outpatient rotation at Methodist Hospital and at general and specialty neurology clinics
Learning: Inpatient consults for acute stroke/TIA, intractable headache, neuromuscular disease, EMG clinic, outpatient management of Parkinson’s and other movement disorders, evaluation of seizures
OBSTETRICS 1
Setting: One month inpatient rotation at Methodist Hospital Family Birth Center with OB/GYN staff
Learning: Triage of patients who require antenatal care, active management of child-birth and labor complications. Additionally, trainees learn obstetrical procedures (such as artificially rupturing membranes, placing internal monitors, repairing lacerations), lactation rounds, perinatology clinic learning about managing patients requiring additional OB care, performing OB ultrasound
OBSTETRICS 2
Setting: One month inpatient rotation at Methodist Hospital Family Birth Center with OB/GYN staff
Learning: Continuation of developing mastery of the same topics from Obstetrics 1
PEDIATRICS 1
Setting: One-month outpatient clinic rotation with pediatricians at Park Nicollet Clinic.
Learning: Acute and well-child care, effective communication with families, health promotion, care for chronic childhood disease, clinic ADHD management
PEDIATRICS 2
Setting: Two weeks of pediatric emergency medicine at Children’s Hospitals and Clinics of Minnesota in Minneapolis, and two weeks of mixed experiences inpatient at Methodist Hospital (Level II nursery care, hospital rounds).
Learning: Pediatric emergency care, management of neonates from at-risk environments in the Level II nursery, management of pediatric patients in a non-specialty hospital, and on rounds with the rounding pediatrician at Methodist Hospital, management of children with neurobiological disorders
SURGERY 1
Setting: One-month rotation of ambulatory surgery at Methodist Hospital
Learning: G1 residents will achieve competence in the diagnosis and management of common surgical problems seen in primary- and secondary-care settings.
Second and third year
CARDIOLOGY 2 (THIRD YEAR)
Setting: One month rotation multiple clinic locations
Learning: Ongoing review of management of cardiac conditions with focus on specialty outpatient conditions such as outpatient management of CHF, management of warfarin dosing, management of dyslipidemia, EKGs, echocardiograms, cardiac imaging
COMMUNITY HEALTH (THIRD YEAR)
Setting: One month rotation, location to be determined by resident's interest
Learning: Residents typically choose one of the following three tracks:
A practice search track in which residents examine a community where they are interested in practicing after residency
An adventure or global track where residents travel to a community of interest to study determinants of that community’s health
A Creekside track where residents select a local population of interest (e.g. LGBTQIA+, adolescents, urban underserved, etc.) and study that community while continuing to see patients at Creekside
ELECTIVE (SECOND/THIRD YEAR)
Setting: Dependent on elective
Learning: Dependent on elective
FAMILY MEDICINE CLINIC (THIRD YEAR)
Setting: One month
Learning: Through the provision of continuity care for patients in a model clinic, residents will gain an understanding of the full spectrum of diseases and conditions that are present in general family medicine, and will understand essential practice management tools which will enable them to graduate from residency ready to practice as effective clinicians.
FAMILY MEDICINE INPATIENT (SECOND YEAR/THIRD YEAR)
Setting: One month (second year) and two months (third year) rotation at Creekside
Learning: Ongoing integrative care in the outpatient clinic setting, developing mastery of the breadth of topics required by a family medicine physician, care for everyone for everything. Residents act as the senior on service during their third year and are in charge of managing the service and facilitating learning for junior residents.
GASTROENTEROLOGY
Setting: One month mixed inpatient/outpatient experience with gastroenterology staff
Learning: Hospital management of acute GI bleeds, cirrhosis, hepatitis, and diarrhea. Clinic management of Inflammatory bowel disease, irritable bowel syndrome, GERD, and peptic ulcer disease. Participation in endoscopy/colonoscopy.
GYNECOLOGY (SECOND/THIRD YEAR)
Setting: One month outpatient rotation at various clinic sites throughout Park Nicollet with OB/GYN and urogynecology staff
Learning: Common topics include contraceptive management and counseling, management of abnormal Pap smears/HPV tests, common office GYN procedures, urinary incontinence, sexual health topics, management of meno/metrorrhagia, evaluation of abnormal vaginal bleeding, management of cystocele/rectocele
HEMATOLOGY / ONCOLOGY / PALLIATIVE CARE / HOSPICE
Setting: One month mixed inpatient/outpatient rotation at Methodist Hospital and community clinics with hematology/oncology, palliative care, and hospice care staff
Learning: Inpatient management of complications of oncologic disease, management of pain and suffering, end-of-life care discussions, family conferences, fundamentals of hospice care
INFECTIOUS DISEASE (SECOND YEAR)
Setting: One month
Learning: Residents will gain an understanding of hospital infectious diseases that is frequently present in patients on a family medicine service and may be referred to as an infectious disease consultant.
OBSTETRICS 3 (SECOND YEAR)
Setting: One month
Learning: Residents will gain an in-depth understanding of maternity care, labor and delivery, postpartum care, and of the roles of the family physician and obstetrician as partners in the care of pregnant patients.
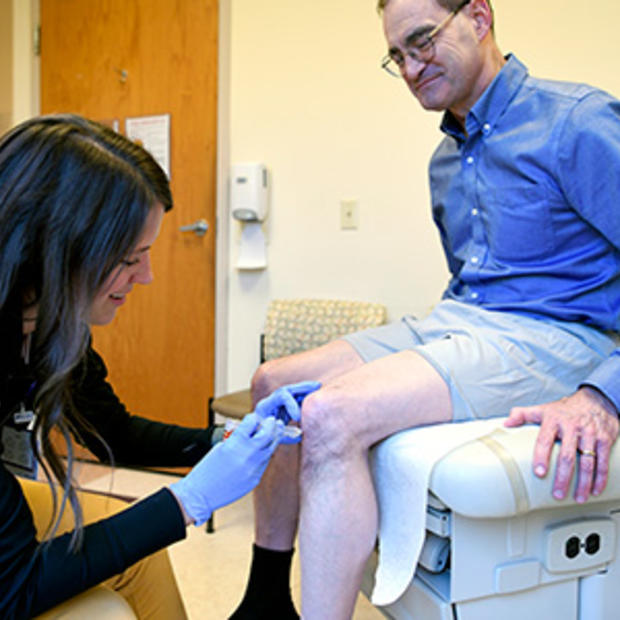
ORTHOPEDICS 1 (SECOND YEAR)
Setting: One month outpatient rotation at the TRIA acute orthopedic injury clinic in with orthopedic staff (includes CAQ sports medicine family physicians)
Learning: Evaluation and management of acute orthopedic injuries, joint injections, casting, splinting
ORTHOPEDICS 2 (THIRD YEAR)
Setting: One month rotation at the orthopedic clinic with orthopedic surgery staff
Learning: Clinic evaluation and management of common orthopedic concerns, casting, splinting
PEDIATRICS 3 (SECOND YEAR)
Setting: One month inpatient rotation at Children’s Hospitals and Clinics of Minnesota with attendings, pediatricians, and medicine and pediatrics senior residents
Learning: Hospital management of acutely ill pediatric patients, RSV bronchiolitis, rotavirus infections, neonatal febrile illness, asthma exacerbations, post-streptococcal glomerulonephritis, seizure disorders, and other common presenting concerns
PEDIATRICS 4 (THIRD YEAR)
Setting: One month outpatient rotation at Park Nicollet Clinic - Shakopee with pediatricians
Learning: Continuing developing mastery of outpatient pediatric care, option for spending time in pediatric subspecialty clinics
PSYCHIATRY (SECOND/THIRD YEAR)
Setting: Two month longitudinal rotation in the G2 or G3 years at Creekside
Learning: Evaluation and management of presenting psychiatric concerns, including depression, anxiety, OCD, panic disorder, schizophrenia, ADHD, personality disorders, and others
PULMONOLOGY (SECOND YEAR)
Setting: One month mixed inpatient/outpatient experience with pulmonary staff
Learning: Hospital management of pulmonary disease, clinic management of chronic pulmonary disease, asthma, COPD, BOOP, IPF
SUBSPECIALTY ROTATION (SECOND/THIRD YEAR)
Setting: Two months for both second and third year at various locations with Park Nicollet subspecialists
Learning: Dependent on rotation, but generally learning details of medicine specialties as they pertain to primary care. Examples of the subspecialties we rotate with include endocrinology, dermatology, ENT, nephrology, psychiatry, and ophthalmology.
Elective opportunities
- Addiction Medicine
- Eating Disorders
- Gender
- Hospitalist
- Nutrition
- Obstetrics
- Palliative Care
- Parental
- Pharmacotherapy
- Procedures
- Rheumatology
- Reproductive Choice / Abortion Training
- Urgent Care
- Weight Management
Methodist Behavioral Medicine Curriculum
Behavioral medicine is integrated longitudinally into the resident experience, including:
- Diagnosing and treating mental illness
- Honing communication skills and interviewing techniques
- Developing self-awareness and mutual support among residents and faculty
Faculty
Behaviorist
- Provides psychotherapy for patients
- Supervises social work students
- Coordinates and leads resident video reviews
- Presents noon conferences
- Shadows first-year residents in the clinic and hospital
- Spends time in the preceptor room, helping with psychosocial concerns
Psychiatrist
- Residents participate in his practice on their psychiatry rotation
- Presents noon conferences
- Available to precept psychiatric care in clinic and arranges for "co-visits"
- Residents have co-visits with the psychiatrist evaluating continuity patients in clinic
Communication skills
- Resident-patient interactions are directly observed by faculty and reflected on through video recording
- Noon didactic presentations cover interviewing techniques, end-of-life issues, adolescent health, and family life cycles
- Faculty observe history and physical exams on patients admitted to the hospital
- Reflection groups provide an opportunity to discuss difficult patients
Support and reflection groups
- First-year residents meet twice monthly with behaviorist and family physicians to discuss stress management and professional formation
- Residents participate in three reflection meetings per year to address issues of meaning and offer opportunities to discuss difficult patients (facilitated by faculty)
- Annual retreats provide guidance for the upcoming year
- Faculty advisors meet quarterly with residents to review academic progress and assess well-being
- The hospital offers Schwartz Center Rounds, a multidisciplinary forum to discuss social and emotional issues that arise caring for patients
Methodist Community Health Curriculum
- Independently assess community, environmental, and family influences on the health of patients
- Be responsive to the larger context and system of health care
- Call effectively on other resources in the system to provide optimal health care.
Longitudinal curriculum
- Factors adding richness to the community health experience:
- Our socioeconomically and culturally diverse clinic population, which includes immigrants and families from around the country and world
- Third-year residents practice at a free walk-in clinic
- Two days at the Minnesota Department of Health, learning about epidemiology and health department services
- Online virtual community-oriented primary care project
Block rotation
Third-year residents participate in a month-long, self-designed community health rotation. Residents define a community, identify the components of community health in that setting and how they are integrated into a family medicine practice. At the conclusion of the month, residents present findings at a noon conference.
Community health course
Each resident attends the Community Health course with other UMN family medicine residents, sponsored by UMN Family Medicine and Community Health. The course focuses on current and historical systems and their sequela that impact the health and wellness of communities. Residents engage in skill building to address these challenges and develop tools for career-long engagement to work with and alongside all the communities we serve.
Methodist Developmental Pediatrics and Adolescent Medicine
Caring for children and youth is an integral part of our mission, taught both longitudinally and in block rotations.
Screening
- Standardized to evaluate infants and children for developmental concerns, autism, and mental health issues
- Teen screens identify psychosocial issues
- Referral sources available
- Active participant in Health Partners' Children's Health Initiative
Patient care
- Adolescent care at Park Nicollet Clinic-Creekside and Central Clinic
Community
- Service required and fulfilled in a variety of ways, including providing school-based sports physicals and screening exams; talking to school groups about health topics; staffing athletic training rooms; tutoring children; and working diabetes or asthma camps
- Committed since 1993 to putting Children First, which encourages the community to work toward increasing the developmental assets of youth
- St. Louis Park routinely listed in the “100 Best Communities for Young People”, thanks in part to the contributions of residents at Central Clinic
Faculty and Patient Care
Faculty
Patient care
Clinic
Park Nicollet Clinic – Creekside serves as a medical home to a large population of independent, older adults.
Residents manage the following:
- Home care
- Rehabilitation services
- Specialty referral
- Interpreting the health care system to maturing patients
Inpatient hospital service
Our inpatient family medicine hospital service usually includes a substantial geriatric population.
- Counsel patients and families about end-of-life issues and work with the care integration team to plan appropriate patient disposition
- Receive training as Physicians Orders for Life Sustaining Treatment (POLST) facilitators to help clarify treatment plans and orders
- Learn a multidisciplinary approach to delirium prevention and treatment, including utilizing the Hospital Elder Life Program to reduce incidence in at-risk patients
Home care, long-term care, and TCU
- Care for panels of four to six nursing home patients during second and third years, and care for TCU patients
- Round monthly with attending and nurse practitioner; topics include behavioral challenges, life cycles, and practice management
- Use innovative Geriatric Tool Kit—the award-winning, resident-designed backpack—to expand services offered in the nursing home
- Call includes taking telephone calls from nursing homes regarding acute changes in patients
- Learn how to manage nursing home patients as part of family medicine practice
Assisted living
- Learn to care for patients in independent senior apartments and an assisted living environment
- Learn how to help promote health and well-being with patients and their families in a home setting
Home visits
Residents assess the homes of older patients as well as health needs in the context of the living environment.
Lead resident duties
Training
The elected lead attends the AAFP Chief Resident Leadership Development Program, an online workshop, and a follow-up workshop at the AAFP Assembly. Expenses are paid by the program.
Administrative responsibilities
- Make call schedule and facilitate coverage in emergencies, illness, or conflicts
- Attend faculty meetings and retreats when appropriate and serve as spokesperson for residents
- Coordinate and run the monthly open resident meeting and closed resident meeting when assistant lead is not available
- Attend monthly nursing meetings or coordinate coverage with assistant lead
- Assist residency coordinator with recruitment activities
- Provide input on policy development
- Orient the newly elected lead in preparation for the coming year
- Foster team building and cooperation among residents through occasional organized social activities or other events as needed
Other expectations
- Maintain full academic responsibilities and remain in good academic standing
- Adapt to the changing needs of the residency
Assistant lead duties
The assistant lead works closely with the clinic medical director and manager as well as the residency coordinator and director regarding resident concerns, residency requirements, and practice management issues. The assistant lead works in conjunction with the elected third-year lead resident. The assistant lead role coincides with the third-year subspecialty rotation.
Evaluation
- Continuous feedback throughout training
- Quarterly meetings with faculty advisor to review progress and academic/career goals, milestone-based evaluations on rotations, and feedback from clinic staff, patients, peers, and faculty
- Semi-annual evaluation by clinical competency committee
- Video review of patient encounters
- "On the fly" feedback while precepting
Call
First year
First-year residents gain experience in evaluating and managing a range of acute medical problems.
OB call is 24 hours averaging every fourth night while on rotation.
House call averages every fifth night until 10:00 p.m.
Responsibilities:
- Rapid initial evaluation of hospitalized patients who have an acute status change
- Residents lead the code team for adult codes
Prerequisites:
- Certification in Advanced Cardiovascular Life Support (ACLS) and Neonatal Resuscitation Program (NRP) will be required during orientation
- Ability to manage critically ill patients (with support from second-/third-year resident on-call)
Second and third year
Second- and third-year residents take overnight call three/four times per month. In addition to house coverage for the hospital, they admit patients to the family medicine service while on call.
Room
- Used exclusively by Methodist residents
- Includes private bathroom and shower, lockers, a Sleep Number bed, a small library, TV, a small refrigerator, and computer access
Methodist Longitudinal Experiences
Our longitudinal experiences include the following:
- Daily noon conferences
- Continuity of patient care
- Curriculum includes:
- Behavioral medicine
- Community health
- Developmental pediatrics and adolescent medicine
- Geriatrics
- Practice management
- Sports medicine with longitudinal athletic training room (optional)