Finding the Root to Treat Aging through Dieting
Researchers at the University of Minnesota Medical School believe they discovered a new way in which diet influences aging-related diseases.
“Our healthcare as we age is analogous to a tree, and the way we go about it now, when a branch gets diseased, we go to a doctor, and they trim the branch. Then, we go to another doctor, and they trim another branch,” said Doug Mashek, PhD, a professor in the Departments of Medicine and Biochemistry, Molecular Biology and Biophysics. “It’s the roots that we need to be focused on—the common roots of all of these diseases. That’s why we are excited because this pathway has been linked to almost all of them. It’s the roots.”
The root is part of a special diet—one that Dr. Mashek and his team have studied over the last eight years with the help of multiple grants from the National Institutes of Health. Their research findings, recently published in Molecular Cell, focus on the Mediterranean diet. The diet, originally touted by U-famed American physiologist Ancel Keys, emerged during his “Seven Countries Study” when he helped link diet to cardiovascular disease for the first time.
Early studies suggested red wine was a major contributor to the health benefits of the Mediterranean diet because it contains a compound called resveratrol, which activated a certain pathway in cells known to increase lifespan and prevent aging-related diseases. However, work in Dr. Mashek’s lab suggests that it is the fat in olive oil, another component of the Mediterranean diet, that is actually activating this pathway.
“We didn’t start out by studying the Mediterranean diet; we first were focusing on fat,” Dr. Mashek said. “This fat is known to be protective against heart disease and many other aging-related diseases, so by identifying this pathway, it provides a new way of thinking about how consuming olive oil and the Mediterranean diet is actually linked to positive health benefits.”
Yet, merely consuming olive oil is not enough to elicit all of the health benefits. Dr. Mashek’s studies suggest that when coupled with fasting, limiting caloric intake and exercising, the effects of consuming olive oil will be most pronounced.
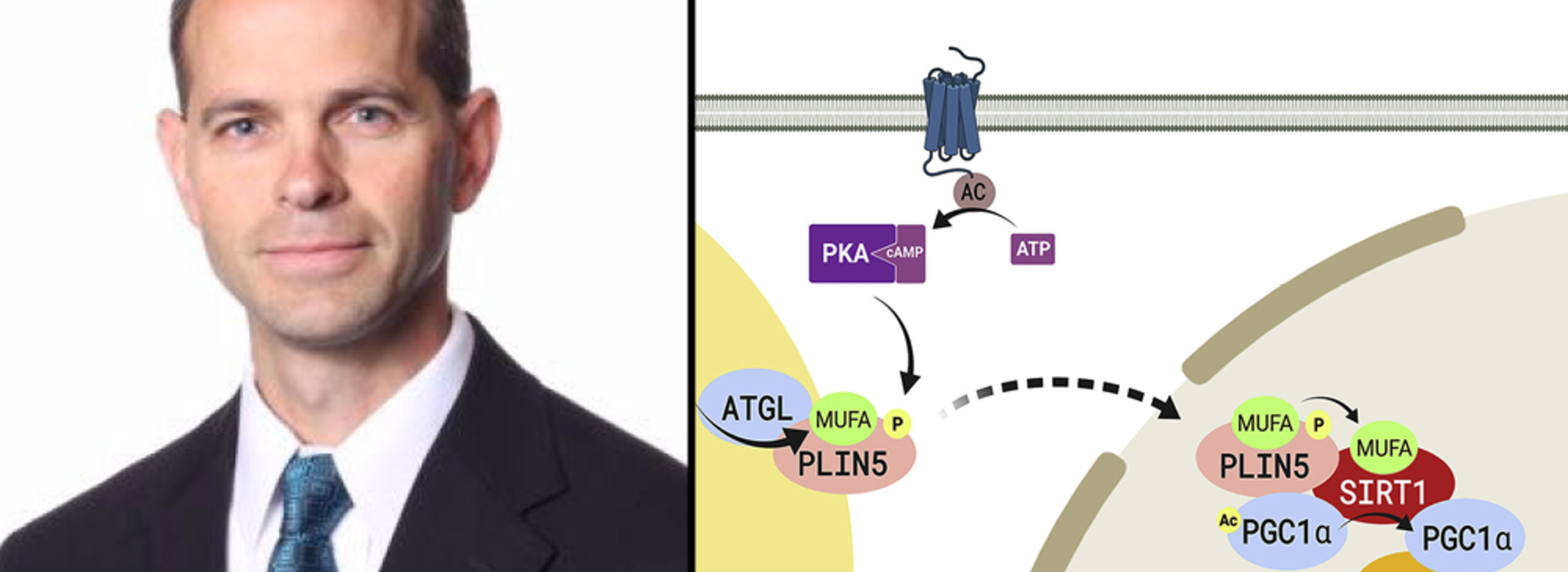
“We found that the way this fat works is it first has to get stored in microscopic things called lipid droplets, which is how our cells store fat. And then, when the fat is broken down during exercising or fasting, for example, is when the signaling and beneficial effects are realized,” he said.
The next steps for their research are to translate it to humans with the goal of discovering new drugs or to further tailor dietary regimens that improve health, both short-term and long-term.
“We want to understand the biology, and then translate it to humans, hopefully changing the paradigm of healthcare from you going to eight different doctors to treat your eight different disorders,” Dr. Mashek said. “These are all aging-related diseases, so let’s treat aging."