
Study establishes the value of cardiovascular magnetic resonance imaging for suspected cardiac tumors
The U of M Medical School study concludes that CMR should be the technique of choice
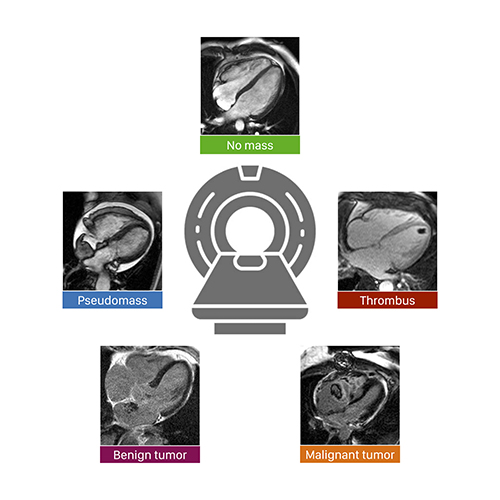
MINNEAPOLIS/ST. PAUL (10/07/2021) - In a first-of-its-kind study, researchers from the University of Minnesota Medical School led a large, multicenter investigation on whether cardiovascular magnetic resonance (CMR) is the best approach in evaluating patients with suspected cardiac tumors. Their results prove that CMR provides high accuracy and prognostic value for this purpose.
“This was important to study because, until now, there was no great data supporting current clinical practice of using CMR to investigate these patients,” said lead author Chetan Shenoy, MBBS, MS, an associate professor in the Department of Medicine’s Cardiovascular Division at the U of M Medical School. “For example, if CMR shows no cardiac tumor or mass, we do not do any further testing — we do not know if this is the right approach and how well CMR serves this purpose. In this study, we wanted to validate that clinical practice.”
This multicenter study, published in the European Heart Journal, involved 903 patients from four institutions. Some of the key findings of the study are that:
-
CMR diagnosis was accurate in 98.4% of patients in the study;
-
CMR diagnosis is a powerful, independent predictor of death; and,
-
This prognostic value is incremental to clinical factors.
“These data provide the first large-scale validation of the clinical practice of using CMR to exclude a cardiac tumor and to diagnose the type of tumor,” said Shenoy, who is also a cardiologist with M Health Fairview. “By demonstrating high accuracy and long-term prognostic value, our results confirm that CMR can be used as a ‘one-stop-shop’ for this clinical indication. We anticipate our findings will shape future guidelines, appropriateness documents and health policies on this topic.”
Co-authors on the paper include John D. Grizzard and Marianna Zagurovskaya from Virginia Commonwealth University Medical Center; Dipan J. Shah, Mahwash Kassi and Michael J. Reardon from Houston Methodist Hospital; and Han W. Kim, Michele A. Parker and Raymond J. Kim from Duke University Medical Center.
This research was funded by the National Institutes of Health (grant K23HL132011) to Chetan Shenoy and (R01HL64726) to Raymond J. Kim.
###
About the University of Minnesota Medical School
The University of Minnesota Medical School is at the forefront of learning and discovery, transforming medical care and educating the next generation of physicians. Our graduates and faculty produce high-impact biomedical research and advance the practice of medicine. We acknowledge that the U of M Medical School, both the Twin Cities campus and Duluth campus, is located on traditional, ancestral and contemporary lands of the Dakota and the Ojibwe, and scores of other Indigenous people, and we affirm our commitment to tribal communities and their sovereignty as we seek to improve and strengthen our relations with tribal nations. For more information about the U of M Medical School, please visit med.umn.edu.
For media requests, please contact:
Angel Mendez
Media Relations Manager
University of Minnesota Medical School
mende434@umn.edu