Dr. Hai-Thien Phu Strives to Make a Difference in COVID-19 Pandemic, and Beyond
Originally from Vietnam, first-year internal medicine and pediatrics resident Hai-Thien Phu, MD, and her family immigrated to Minnesota when she was three years old.
“Minnesota has always been my home,” Dr. Phu said. “I knew that I wanted to stay close to my family during residency. And, frankly, the University of Minnesota has a really good program, so it was the perfect match.”
Residents are incredibly busy. As someone who focuses on two specialties––internal medicine and pediatrics–– Dr. Phu is no exception. She routinely cares for both adults and kids of all ages.
“It’s a dance. Going to work and then home, spending as much time as I can with my husband, Tom, and then repeating the process, day in and day out,” she said. “I am blessed to have accomplished my dreams of becoming a doctor, in no small part to my parents’ sacrifice by giving up their life in Vietnam and immigrating to America, so I can have a good education.”
Striving to Make a Difference
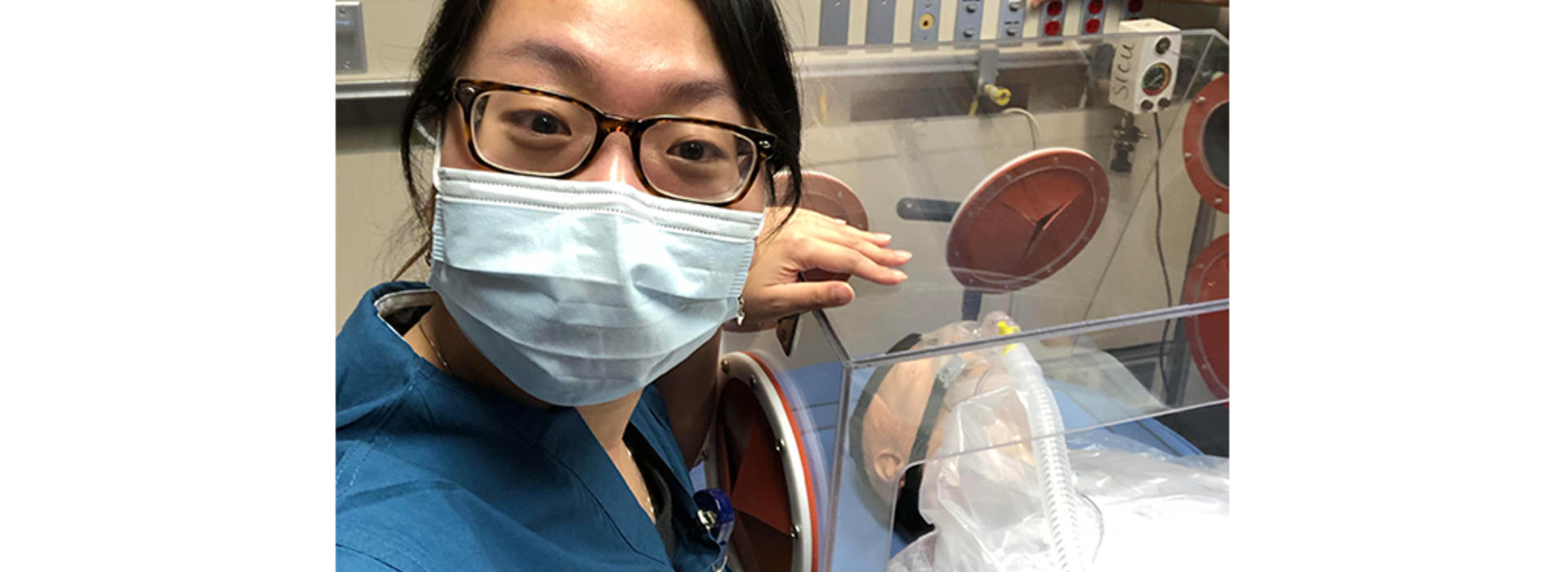
“I think of the COVID-19 pandemic as a partnership between everyone––we’re all in this together, right?” she said. “So one day, I was scrolling through social media. And, when I saw the aerosol box designed by Dr. Hsien Yung Lai in Taiwan, I thought, ‘This would make a huge difference, especially with our short supply of PPE.’”
Dr. Phu thought the aerosol box was great as a splash guard, but she felt that it could be useful in other ways, too, like for the use of non-invasive ventilation and compassionate extubation while still protecting healthcare workers.
“What if, instead of creating new ventilators, or hooking people up to multiple ventilators, we can use respiratory support devices we’ve always had? With the aerosol hood, we can fully employ non-invasive ventilation (HFNC, CPAP/BiPAP) that have always been used and have worked for our patients in the past.”
This project highlights the phenomenal innovation and collaboration seen at the U of M. “Dr. Asish Abraham has played a significant role in the success of this project,” she said. “Our collaborators from the Mechanical Engineering Department, Ian Marabella, Yensil Park and Austin Andrews, have worked tirelessly to produce and test this device.” Professors Chris Hogan, Kumar Belani, MD, and Gwen Fischer, MD, have all been wonderful mentors, providing guidance based on their areas of expertise.
In addition to non-invasive ventilation, Dr. Phu, along with her colleagues in the Medical School and the College of Science and Engineering’s Department of Mechanical Engineering, are also working on a solution for compassionate extubation––when patients are nearing the end of their lives, and the families are focused on comfort care to allow the patient to pass without pain.
Moving Past the Pandemic
Dr. Phu believes that this device is relevant not only for the COVID-19 pandemic but for all other airborne diseases that come after the pandemic as well.
“According to the NIOSH engineering control guidelines, which demonstrate how to best protect the healthcare field during communicative diseases, PPE is actually the last line of defense,” she said. “For instance, with airborne diseases (like COVID-19), establishing changes across the healthcare system itself, whether that be improving or creating airborne isolation rooms or negative pressure rooms, is much more impactful than the last step––which is PPE.”
Dr. Phu believes that this changes a lot in terms of how we will move forward with pandemics.
“I think this is going to be especially relevant in the decades to come because we are seeing more and more of these airborne viral diseases emerge,” she said. “We need to protect our patients and our healthcare workers, effectively.”