Respirator Safety Shield Protects Physicians, Patients During COVID-19
Just days after the state government enacted a stay-at-home order and hospitals began prepping for COVID-19’s impact, a group of physicians at the University of Minnesota Medical School were looking for innovative ways to improve safety in patient care during the pandemic.
Gwenyth Fischer, MD, recognized that there could be gaps in protection from the virus for frontline healthcare workers. “It became pretty clear to me when we started preparing for COVID-19 that we needed something better to protect us in the field,” said Dr. Fischer, an assistant professor in the Department of Pediatrics.
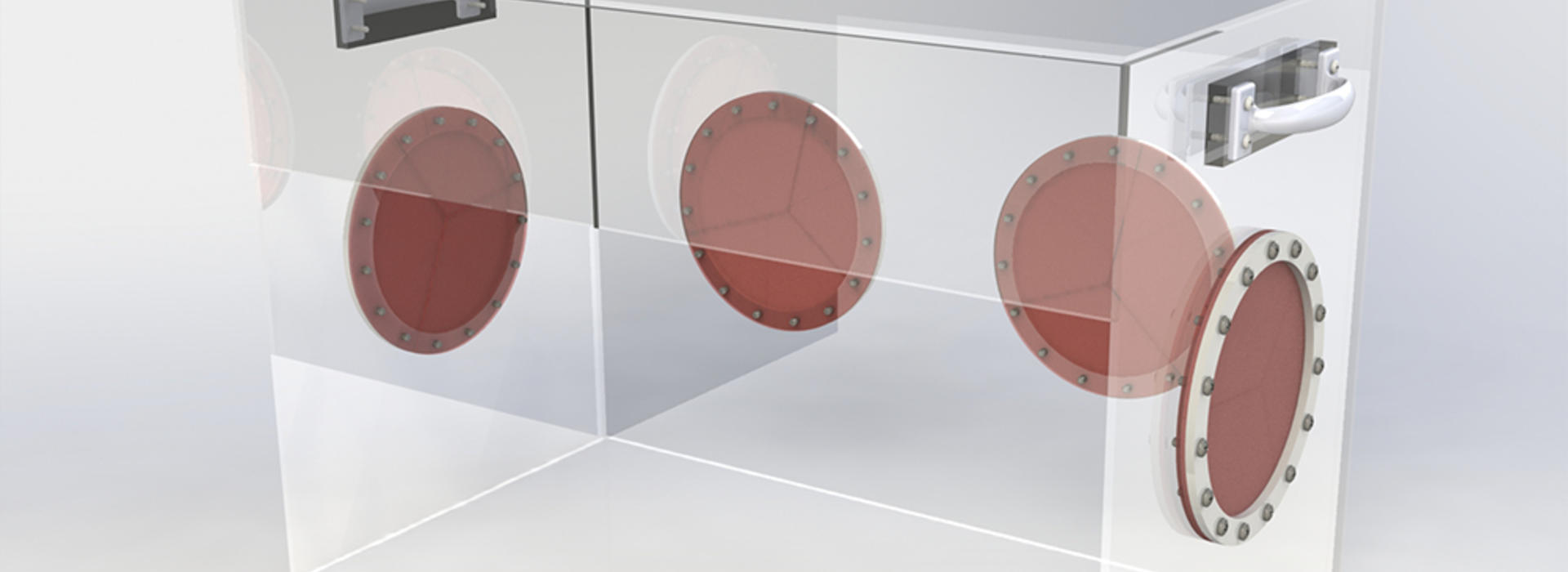
Hai-Thien Phu, MD, a resident in medicine-pediatrics, saw an example from Taiwan and brought it to Dr. Fischer and Asish Abraham, MD, a resident in the Department of Anesthesiology. The device, which served as a respirator safety shield, was a simple but effective box that could be placed around a patient’s head and neck area to work as a splash guard to prevent the spread of contaminated particles.
The group submitted an application for one of the Campus Public Health Officer’s COVID-19 Rapid Response Grants to develop their own respirator safety shield. The grants were implemented in March and aim to catalyze small-scale research projects designed to address and mitigate the risk associated with the COVID-19 pandemic.
Making Improvements
The original Taiwanese design was crude, and the team needed to enhance several features of the device and make it more efficacious. Thankfully, Chris Hogan, PhD, a mechanical engineer in the College of Science and Engineering who also happens to be an expert in aerosol and particle removal, stepped in to help.
The team brought in Kumar Belani, MD, a professor in the Department of Anesthesiology, who helped with the testing process. From the beginning, Dr. Belani knew that the respirator safety shield had limited use to serve just as a barrier, but if properly modified, had great potential. Drs. Belani, Fischer, Phu, Abraham and Hogan figured out that the unit needed to be more than just a physical barrier. They concluded that it would help if it also served the purpose of removing exhaled air, aerosols and droplets around a patient’s breathing areas.
Resources at the University, including the ability to test on-site with the permission of Mojca Konia, MD, PHD, MACM, director of the Simulation Program’s new education center, allowed them to make incremental improvements based on quick feedback.
“We worked with the simulation center and Dr. Janet Hume, who came up with the idea of using ‘glo-germ’ during testing. ‘Glo-germ’ allowed us to see which particles in the box were contaminated while we simulated breathing,” Dr. Fischer said.
Dr. Belani added, “After some head scratching, we decided to install a HEPA filter at the top of the box so it would take any particles inside the system through a filtration mechanism. That was really exciting for us, and we saw the value in it right away."
Over time, the interdisciplinary team added two more holes and several iris ports to the device, and then changed the length and height based on the dimensions of different hospital beds, which can differ between intensive care units (ICU) or regular beds. This adaptive process is called “customer discovery” in the world of medical devices, and it ensures that each device is tailored in a way that delivers results.
How It Helps

When available, personal protective equipment (PPE) is the first line of defense for healthcare workers, and it remains crucial to limiting the spread of the virus. In instances when PPE isn’t available, the patient isolation unit can provide another option for hospitals that are already strained for resources. This translates well to resource-limited countries throughout the world, demonstrating that U of M innovation has no limits.
“It’s not only important to have a barrier between us and the patient, but even if we might be wearing PPE, you still need to have a splash guard, and this would eliminate the need for the gown and eye protection,” Dr. Belani said. “We hope that with this patient isolation unit, patients would get the benefit of what we routinely do, namely the benefit of non-invasive respiratory therapies without the need for mechanical ventilation. This protective isolation system has multiple values and purposes, and we’ve done rigorous testing. It’s quite robust.”
The respirator safety shield will have utility for all respiratory infections, such as measles or SARS. It could also be used in a variety of settings, from the ICU to regular medical units, and even during patient transport from an ambulance into a hospital.
“I work in ‘medical device,’ and it’s incredible how fast everything is going now,” Dr. Fischer said. “It’s amazing how fast we can actually move when patients’ and providers' lives are on the line.”