Students and Faculty Break Down Barriers to Exercise on Campus and in the Community
Students and Faculty Break Down Barriers to Exercise on Campus and in the Community
Exercise as Medicine advisor Dr. Jennifer Oberstar and medical students Josh Levine and Cyrus Nouraee bring the benefits of exercise to the U of M campus and their patients in the community.
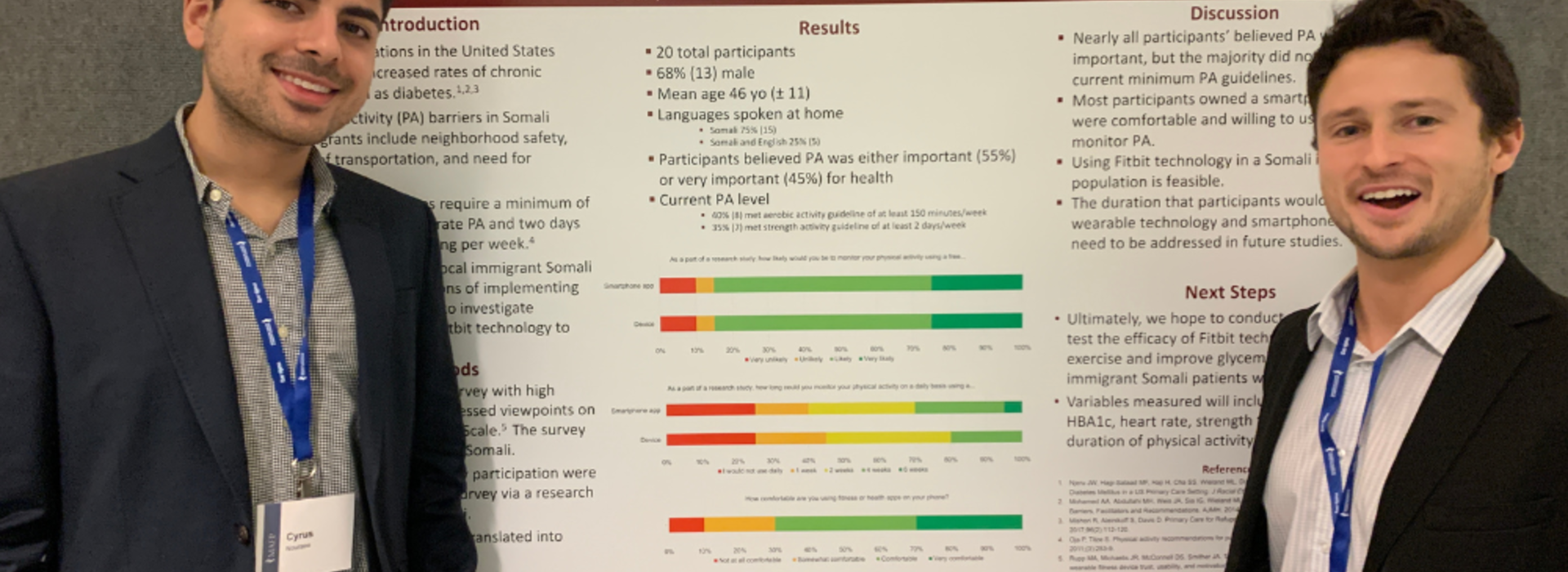
In March, third year U of M medical students Josh Levine and Cyrus Nouraee presented their poster “Activity Perceptions and Fitbit Feasibility Among Somali Immigrants” at the Minnesota Academy of Family Physicians (MAFP) Innovation and Research Forum. They were mentored by Dr. Jennifer Oberstar, advisor for the Exercise is Medicine (EIM) program at the Medical School, and have developed a passion for educating fellow students and their community about the benefits of exercise.
During their first year at the Medical School, all students take the three-part Essentials of Clinical Medicine (ECM) course, which requires learners to engage in a service learning project. Dr. Oberstar, a clinician at the community-based M Health Fairview - Smiley’s in Minneapolis, noticed high rates of diabetes among Somali immigrants and proposed a project addressing the issue for the ECM course in 2019.
“I was interested in it right away, and thought, ‘We’ve got to get on this quickly,’” Levine recalls.
The initial plan for the project was to give wearable fitness trackers, like Fitbits, to Somali immigrant patients at Smiley’s and work with them to develop a personalized fitness plan and track blood sugar and other vitals to measure the impacts of exercise on diabetes control and overall health.
“With the Somali population, and a lot of immigrant populations, there’s a lot of barriers to exercise,” Nouraee explains. “The thinking originally was, can we utilize this technology to help encourage exercise use?”
However, researchers in the Department of Family Medicine and Community Health suggested that, before giving patients devices, the team should first understand the community’s perceptions around fitness trackers.
“There could be ethical concerns just starting to study people with a new technology without really understanding what they think of it,” Levine elaborates. “We needed to understand how feasible the study was.”
Although the students were only required to carry out the project for two semesters, Levine and Nouraee have been working on it for two and half years and are excited to carry the momentum of presenting at MAFP into a published paper, the results of which could be the basis for additional research.
“The big thing that I took away from this project is the numerous meaningful, feasible ways of encouraging exercise in patient populations that have a lot of barriers,” says Nouraee.
Outside of this project, both Levine and Nouraee hope to be models of good exercise habits for their future patients. Levine is currently co-president of the EIM group on campus led by Dr. Oberstar, and the group recently earned a silver star ranking for hosting activities like rock climbing and wheelchair basketball, in addition to educational opportunities for U of M students and the broader Twin Cities community.
“There is evidence that physicians who exercise themselves are more apt to ask their patients of their journey with exercise,” Dr. Oberstar says, emphasizing the importance of getting medical students engaged with physical activity.
Levine and Nouraee point out that their review of the literature showed that exercise lowers all-cause mortality and is especially beneficial for blood sugar, lipid profiles and mental health.
Dr. Oberstar hopes to grow the U of M’s EIM program into a multidisciplinary team and encourage students from all disciplines to prioritize movement. And, as they prepare for their final year as medical students, Levine and Nouraee look forward to promoting exercise in their future practices and finding more opportunities to break down barriers to physical activity.
“I hope to be able to keep providing people with the tools to get all the benefits of physical activity,” says Levine.